SARCOIDOSIS OF THE PERICARDIUM MYOCARDIUM AND LUNG
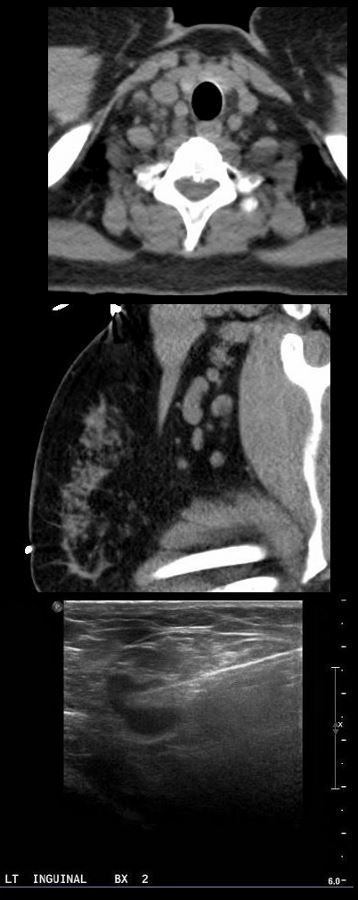
54-year-old female with peripheral adenopathy who had an inguinal node biopsied 6 years prior showing sarcoidosis.
Ashley Davidoff MD
Ashley Davidoff MD
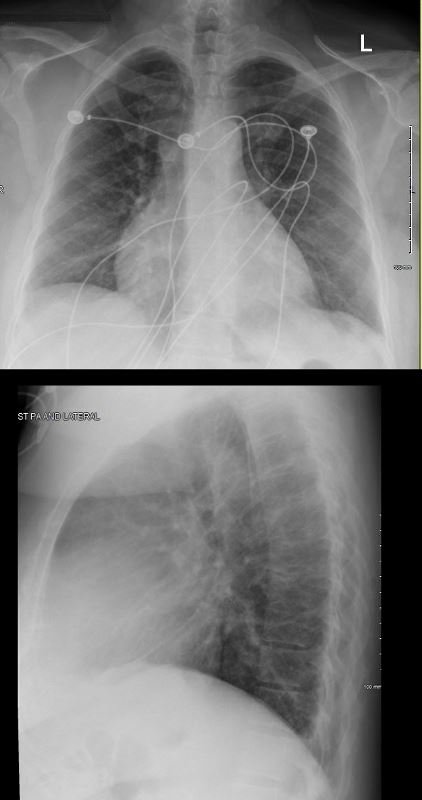
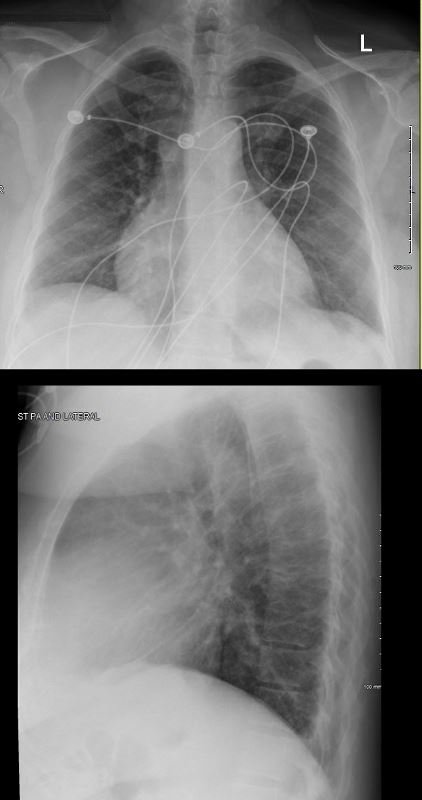
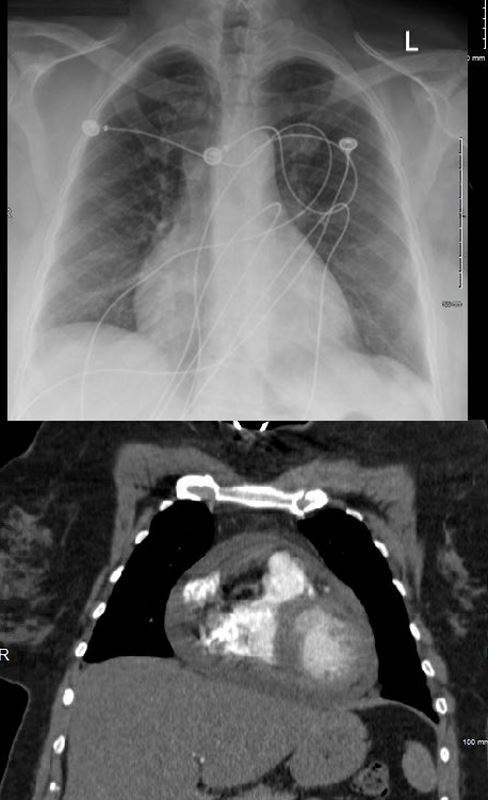
Early Appearance of Pericarditis
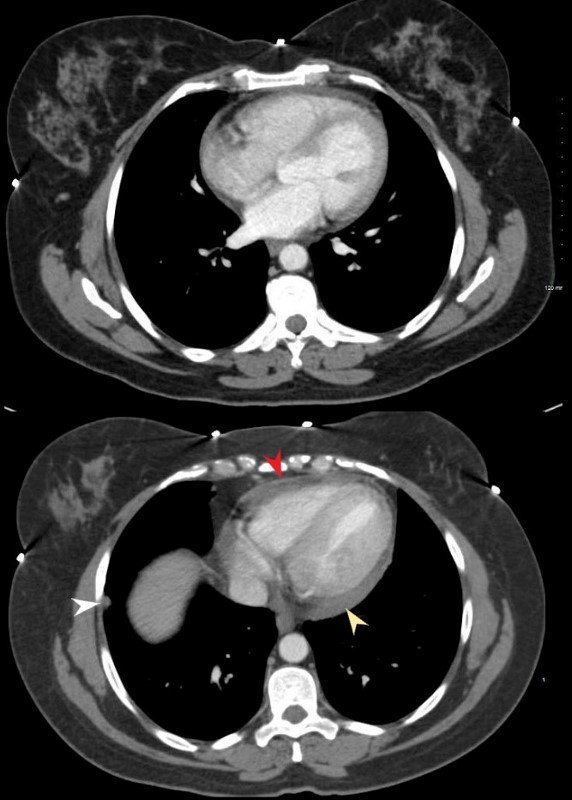
CT shows normal sized chambers s(upper image). The lower image shows mild thickening and irregularity of the pericardium (red arrow head) small effusion (yellow arrowhead) and a pleural nodule (white arrowhead)
She presented with SOB and was noted to have a pericardial effusion by echo without tamponade
Ashley Davidoff MD
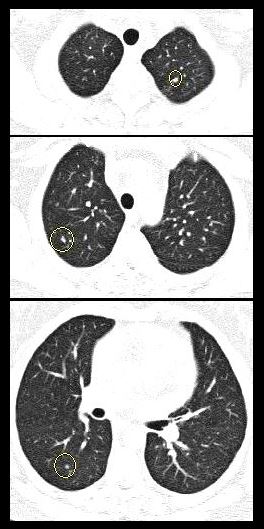
Chest examinations at the time showed little evidence of sarcoid except for a few small nodules. Mild pericardial thickening was present on the CT. She has a history of hypertension COPD; sleep apnea, on CPAP; diabetes mellitus, on metformin; lumpectomy x2; GERD; and vertigo
4 years ago she presented with SOB and was noted to have a pericardial effusion by echo without tamponade
The pericardial effusion was drained with negative cytology and negative for TB . CT at the time following the drainage showed a thickened pericardium with pericardial drain in place
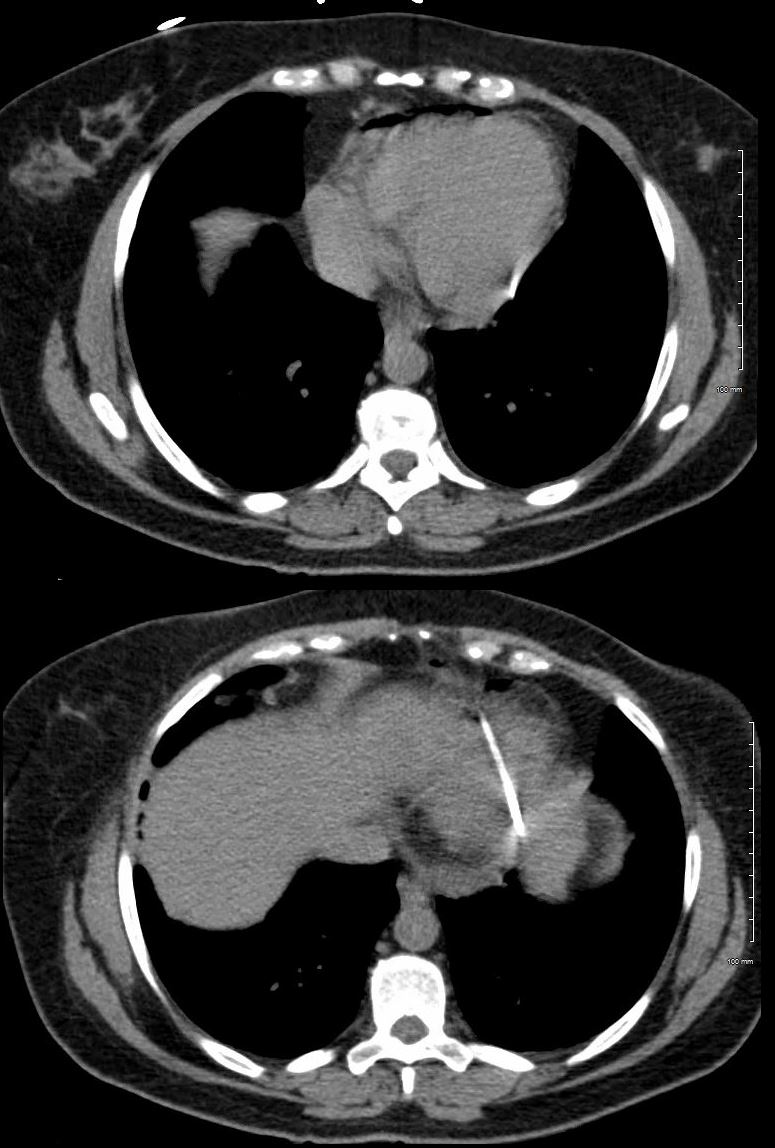
The pericardial effusion was drained with negative cytology and negative for TB . CT at the time following the drainage showed a thickened pericardium with pericardial drain in place
Ashley Davidoff MD
She represented 1 year later with symptoms of worsening intermittent chest pain, and shortness of breath exacerbated with exertion. An echocardiogram, showed recurrent increasing pericardial effusion confirmed by CT. She was placed on steroids but did not tolerate the steroids.
RECURRENT PERICARDIAL EFFUSION CXR,CT CORRELATION
Ashley Davidoff MD
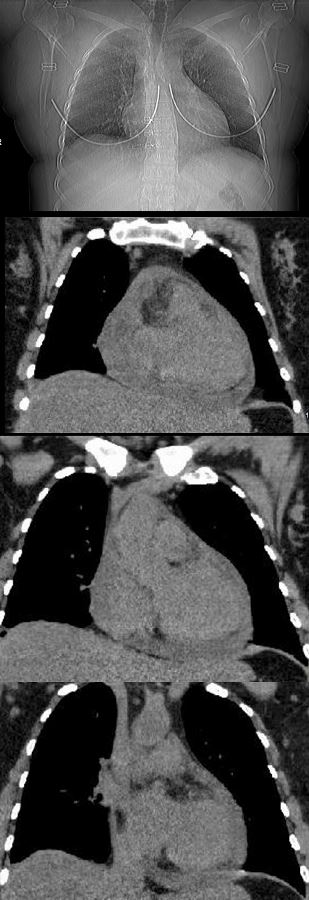
RECURRENT PERICARDIAL EFFUSION
She represented 1 year later with symptoms of worsening intermittent chest pain, and shortness of breath exacerbated with exertion. An echocardiogram, showed recurrent increasing pericardial effusion confirmed by CT.
Ashley Davidoff MD

RECURRENT PERICARDIAL EFFUSION
Ashley Davidoff MD
RECURRENT PERICARDIAL EFFUSION
Ashley Davidoff MD
Later in that year she had another recurrence of pericardial effusion
Ashley Davidoff MD
Ashley Davidoff MD

RECURRENT PERICARDIAL EFFUSION CXR,CT CORRELATION
The lateral examination soft pericardial effusion layering dependently and posteriorly.
Ashley Davidoff MD
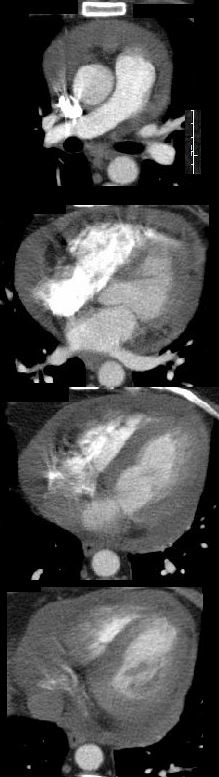
RECURRENT PERICARDIAL EFFUSION NORMAL SIZED CARDIAC CHAMBERS
Ashley Davidoff MD
She underwent surgery for pericardial window and VATS biopsy of her left lower lobe. Her pericardium was noted to be thickened
Pathology revealed Non-necrotizing granulomatous inflammation involving pulmonary interstitium and occasional airways; AFB, GMS, and PAS stains were negative for micro-organisms.
The left pericardial biopsy showed diffuse and extensive non-necrotizing granulomatous inflammation and AFB, GMS, and PAS stains were negative for micro-organisms.
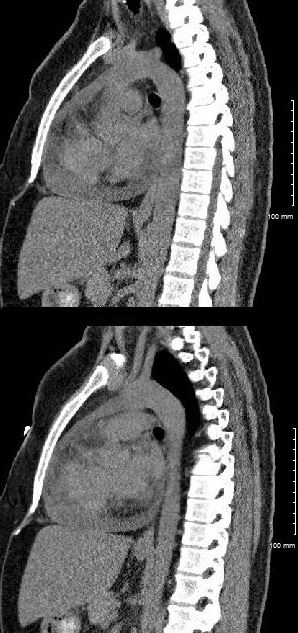
CT scan at the end of that year (131555) showed thickened pericardium.
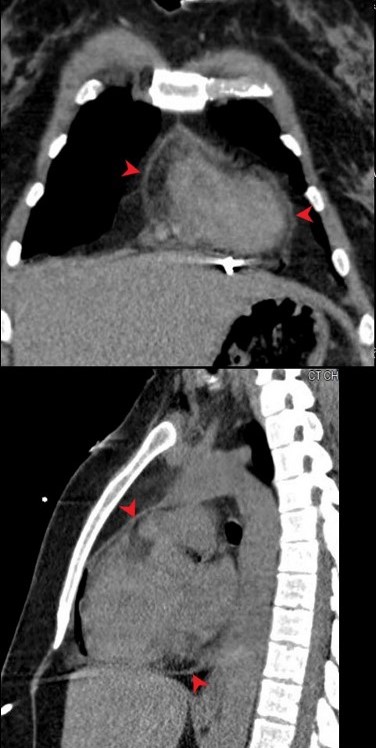
Red arrowheads in the upper and lower images show the thickened pericardium.
The pericardial effusion was drained with negative cytology and negative for TB . CT at the time following the drainage showed a thickened pericardium with pericardial drain in place
Ashley Davidoff MD
2 Months Later No Recurrence of Effusion, but Persistent Pericardial Thickening
CT shows thickening and irregularity of the pericardium
Ashley Davidoff MD
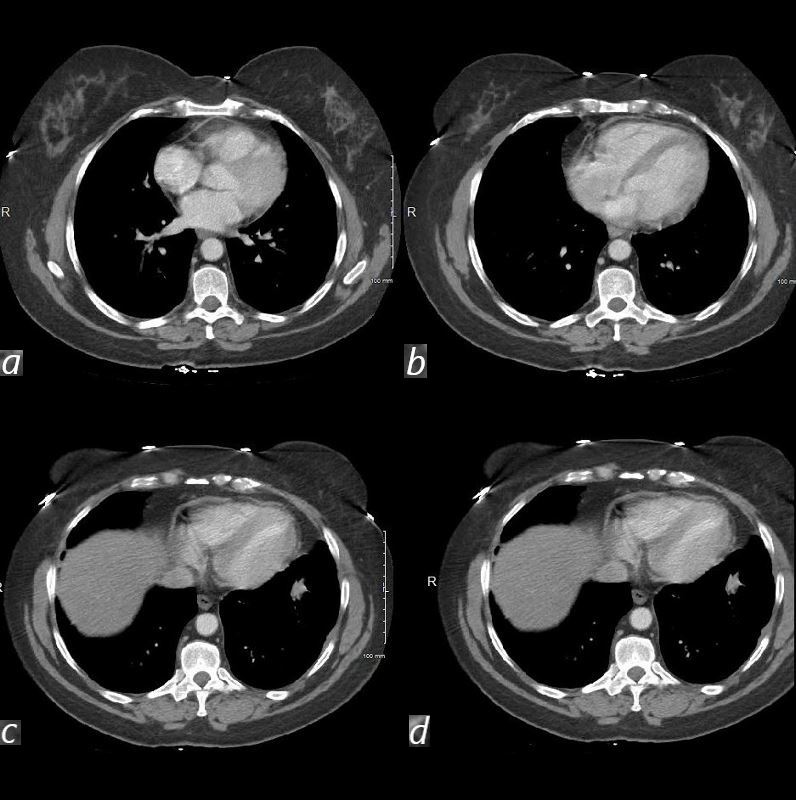
CT from the level of the left atrium (a) threough the right atrium, right ventricle and left ventricle (b), the inferior aspect of the heart, (c) and throuh the inferior vena cava, shows thickening of the pericardium, normal sized cardiac chambers, but no evidence to suggest constriction, withnormal sized IVC.
54-year-old female with peripheral adenopathy who had an inguinal node biopsied 6 years prior showing sarcoidosis. Who chest examinations at the time showed little evidence of sarcoid except for a few small nodules. She has a history of hypertension COPD; sleep apnea, on CPAP; diabetes mellitus, on metformin; lumpectomy x2; GERD; and vertigo
4 years ago she presented with SOB and was noted to have a pericardial effusion by echo without tamponade
The pericardial effusion was drained with negative cytology and negative for TB . CT at the time following the drainage showed a thickened pericardium with pericardial drain in place
She represented 1 year later with symptoms of worsening intermittent chest pain, and shortness of breath exacerbated with exertion. An echocardiogram, showed recurrent increasing pericardial effusion confirmed by CT. She was placed on steroids but did not tolerate the steroids.
Later in that year she underwent surgery for pericardial window and VATS biopsy of her left lower lobe. Her pericardium was noted to be thickened
Pathology revealed Non-necrotizing granulomatous inflammation involving pulmonary interstitium and occasional airways; AFB, GMS, and PAS stains were negative for micro-organisms.
The left pericardial biopsy showed diffuse and extensive non-necrotizing granulomatous inflammation and AFB, GMS, and PAS stains were negative for micro-organisms.
CT scan at the end of that year (131555) showed thickened pericardium.
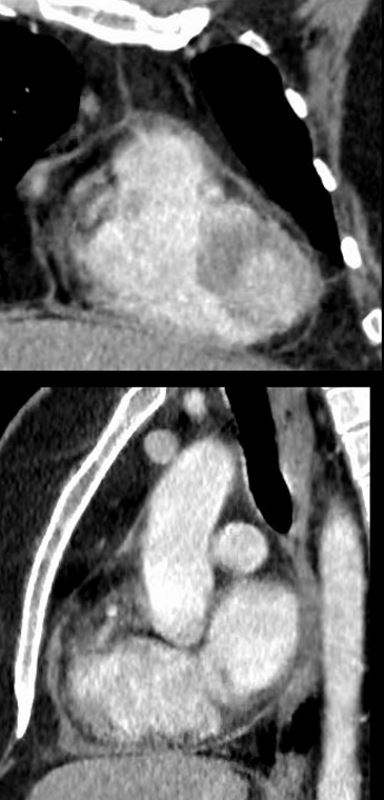
An MRI at the time showed diffuse thickening of the pericardium with enhancement as well as nodular mid myocardial changes at the hinge points and the inferolateral aspects. Subendocardial changes were also noted.
Repeat MRI the next year showed similar findings
Ashley Davidoff MD
An MRI at the time showed diffuse thickening of the pericardium with enhancement as well as nodular mid myocardial changes at the hinge points and the inferolateral aspects. Subendocardial changes were also noted.
Repeat MRI the next year showed similar findings
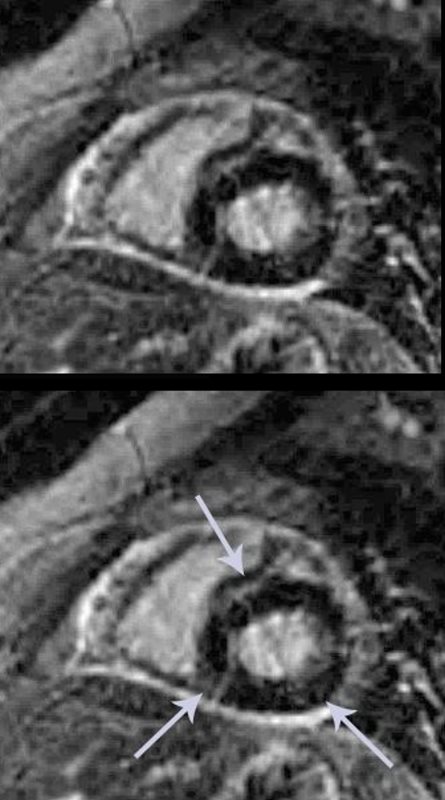
The short axis LGE sequence shows nodular and diffuse heterogeneous LGE in the anteroseptal region, inferoseptal region at the hinge points, and nodular changes in the mid myocardial region of the inferior wall (white arrows) . Extensive pericardial enhancement is also noted
Ashley Davidoff MD
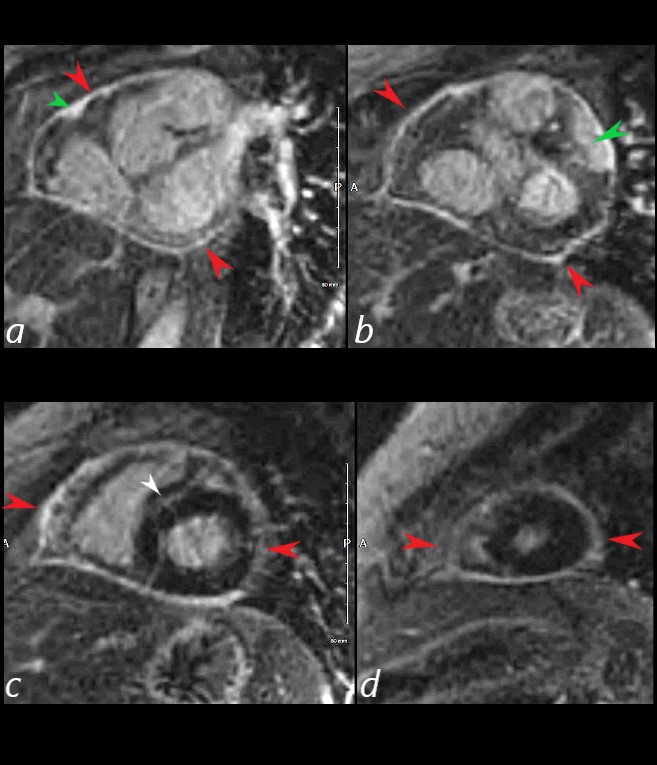
The short axis LGE sequence starting at the base of the heart (a, b) progressing through the body c and apex (d) shows focal LGE in the RVOT(a, green arrowhead) and in the LV (b green arrowhead) extensive pericardial enhancement (a,b,c,d – red arrowheads, and in the septum (white arrowhead c).
Ashley Davidoff MD
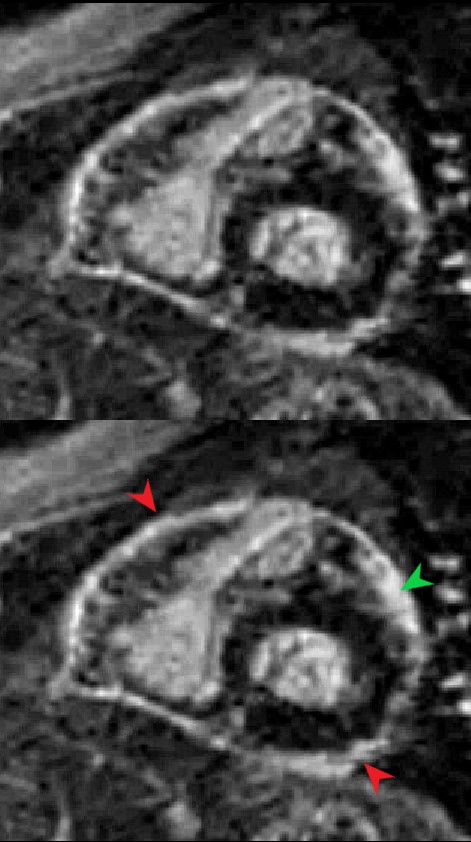
The short axis LGE sequence shows focal diffuse subepicardial LGE (green arrowhead) Extensive pericardial enhancement is also noted (red arrowheads).
Ashley Davidoff MD
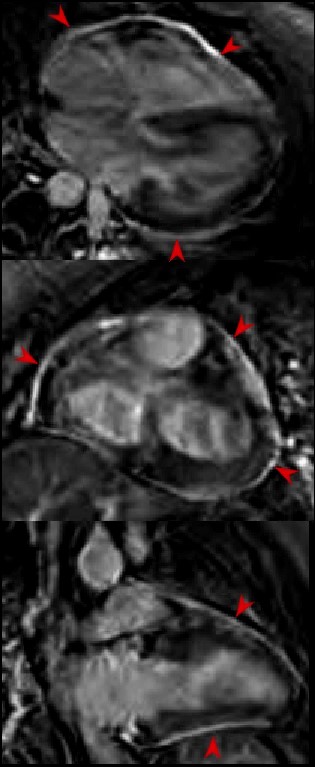
The 4chamber (top image), 3 chamber (middle image) and 2 chamber (lower image) LGE sequences show extensive pericardial enhancement (red arrowheads).
54-year-old female with peripheral adenopathy who had an inguinal node biopsied 6 years prior showing sarcoidosis. Who chest examinations at the time showed little evidence of sarcoid except for a few small nodules. She has a history of hypertension COPD; sleep apnea, on CPAP; diabetes mellitus, on metformin; lumpectomy x2; GERD; and vertigo
4 years ago she presented with SOB and was noted to have a pericardial effusion by echo without tamponade
The pericardial effusion was drained with negative cytology and negative for TB. CT at the time following the drainage showed a thickened pericardium with pericardial drain in place
She represented 1 year later with symptoms of worsening intermittent chest pain, and shortness of breath exacerbated with exertion. An echocardiogram, showed recurrent increasing pericardial effusion confirmed by CT. She was placed on steroids but did not tolerate the steroids.
Later in that year she underwent surgery for pericardial window and VATS biopsy of her left lower lobe. Her pericardium was noted to be thickened
Pathology revealed Non-necrotizing granulomatous inflammation involving pulmonary interstitium and occasional airways; AFB, GMS, and PAS stains were negative for micro-organisms.
The left pericardial biopsy showed diffuse and extensive non-necrotizing granulomatous inflammation and AFB, GMS, and PAS stains were negative for micro-organisms.
CT scan at the end of that year (131555) showed thickened pericardium.
An MRI at the time showed diffuse thickening of the pericardium with enhancement as well as nodular mid myocardial changes at the hinge points and the inferolateral aspects. Subendocardial changes were also noted.
Repeat MRI the next year showed similar findings
Ashley Davidoff MD
She represented 1 year later with symptoms of worsening intermittent chest pain, and shortness of breath exacerbated with exertion. An echocardiogram, showed recurrent increasing pericardial effusion confirmed by CT. She was placed on steroids but did not tolerate the steroids.
Later in that year she underwent surgery for pericardial window and VATS biopsy of her left lower lobe. Her pericardium was noted to be thickened
Pathology revealed Non-necrotizing granulomatous inflammation involving pulmonary interstitium and occasional airways; AFB, GMS, and PAS stains were negative for micro-organisms.
The left pericardial biopsy showed diffuse and extensive non-necrotizing granulomatous inflammation and AFB, GMS, and PAS stains were negative for micro-organisms.
CT scan at the end of that year (131555) showed thickened pericardium.
An MRI at the time showed diffuse thickening of the pericardium with enhancement as well as nodular mid myocardial changes at the hinge points and the inferolateral aspects. Subendocardial changes were also noted.
Repeat MRI the next year showed similar findings
