Function
Ganesh Athappan MD Ashley Davidoff MD
Introduction
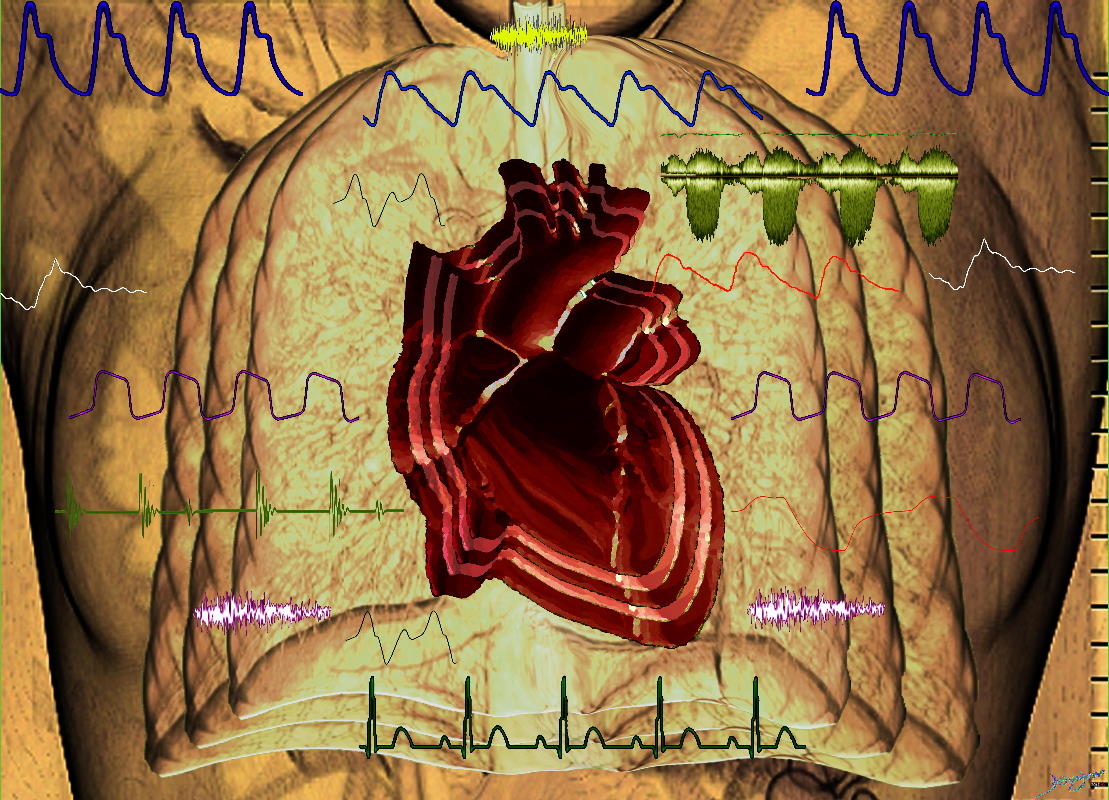
Ashley Davidoff MD TheCommonVein.net
heart-0112
Systole and Diastole
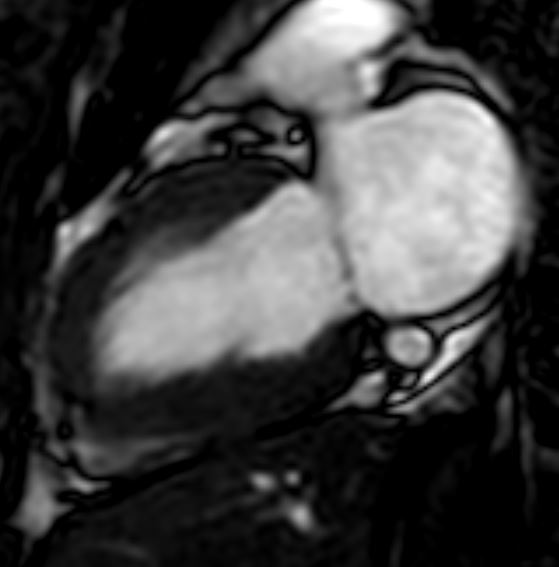
The parasagittal view through the left atrium and left ventricle shows the heart in peak (end) systole with closed mitral valve
Ashley Davidoff TheCommonVein.net MRI normal 001
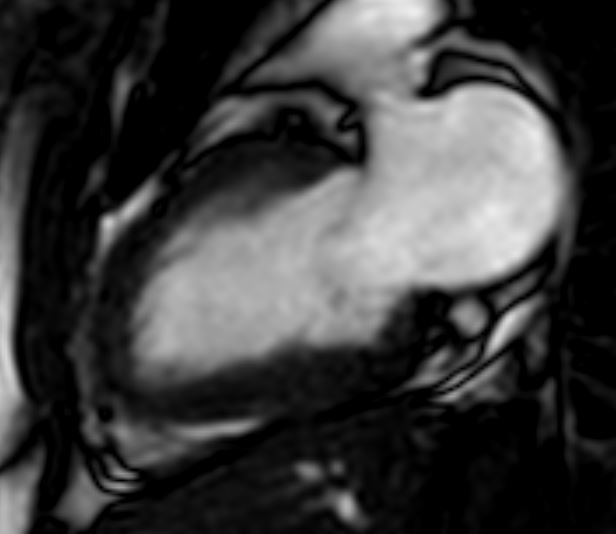
The parasagittal view through the left atrium and left ventricle shows the heart in early diastole with open mitral valve
Ashley Davidoff TheCommonVein.net MRI normal 002
The parasagittal view through the left atrium and left ventricle shows the heart in end diastole with closed mitral valve
Ashley Davidoff TheCommonVein.net MRI normal 003
The axial view through the left atrium and left ventricle shows the heart in peak (end) systole with closed mitral valve
Ashley Davidoff TheCommonVein.net MRI normal 003
The axial view through the left atrium and left ventricle shows the heart in early diastole with open mitral valve
Ashley Davidoff TheCommonVein.net MRI normal 004
The axial view through the left atrium and left ventricle shows the heart in end diastole with closed mitral valve
Ashley Davidoff TheCommonVein.net MRI normal 005
The cardiovascular system is the transport system for blood. It is composed of a pump (the heart), a series of distributing and collecting tubes (arteries and veins) and an extensive system of thin vessels for rapid exchange between the tissues and the vascular channels (the capillaries) ,that together form two closed delivery systems of blood vessels, the pulmonary and systemic circulations. The flow of blood through the heart is unidirectional and that through all organs is passive and occurs only because arterial pressure is kept higher than venous pressure by the pumping action of the heart (alternate contraction and relaxation).The right heart pump provides the energy necessary to move blood through the pulmonary vessels, and the left heart pump provides the energy to move blood through the systemic organs.
In fact, it is not just a pump that pumps in and out. There is second to second, and beat to beat variation so that it continuously changes its patterns of contraction and relaxation, always accommodating bodily needs. It has two receiving chambers, the left and right atria, and two dominantly pumping chambers, the left and right ventricles. All biological systems function with similar basic mechanisms. They receive a product, process it, and then export the product. The function of the heart is to receive deoxygenated blood from the systemic circulation, process it by positioning an optimal volume in the ventricles, and then transporting it to the lungs for oxygenation and other body tissues for delivery of metabolic substrates. The right atrium receives deoxygenated blood at low pressure, 0-5 mmHg (millimeters Mercury) transports it through the tricuspid valve into the right ventricle, which generates systolic pressures of 20-25mmHg to result in a more forceful trip through the lungs. The oxygenation process has to be rapid and efficient as the deoxygenated blood whizzes through the capillary system of the alveoli. Once this is accomplished the pressure to reach the left atrium has decreased to barely positive numbers at 1-10mmHg and the left atrium prepares the blood, so that the beat to beat volume of blood that the left ventricle is going to receive is optimized. The blood flows in two waves through the mitral valve – one a passive mechanism caused purely by a differential pressure between the left atrium and the left ventricle during the earliest phases of diastole, and a second active phase during the latter phase of ventricular diastole. In basal conditions, the passive phase accounts for most of the flow into the ventricles. During the active phase there is actually a contraction of the left atrium to enable a “topping up” of the left ventricle just before it begins its systolic phase. The left ventricle is then called upon to generate systolic pressure, normally between 100-120 mmHg. Under basal or resting conditions the active contraction phase accounts for about 30% of ventricular filling. During exercise, the passive phase is shortened due to the rise in heart rate, and the active phase plays a greater role in the filling of the ventricle.
The manner in which the myocytes are arranged for optimal performance is quite an ingenious trick of nature. With about 15% myocyte shortening the heart can eject between 55-65% of its load. In the mid body the cells are circumferentially arranged and are twisted one way under the subendocardium and twisted the opposite way below the epicardium. During systole this allows for shortening in both the axil plane and along the long axis as well as allowing for a wringing or twisting type action to the pattern The base moves clockwise and the apex moves counterclockwise. This type of action, not only allows for efficient emptying but also is thought to have a vacuum effect as relaxation occurs.
The two circulations are connected in series, such that (1) blood from the right atrium, flows to the right ventricle, which pumps it through the vessels of the lungs—the lesser (pulmonary) circulation—to the left atrium and left ventricle and (2) blood from the left ventricle is pumped, into the aorta and its branches to systemic organs and eventually back to the right atrium by way of venous channels – the major (systemic) circulation.
The circulatory system can thus be viewed as a system of conduits (blood vessels) arranged in series and in parallel(individual component s of the systemic circulation) to carry blood.
Blood, the specialized fluid transported by the circulating system, consists of red blood cells, white blood cells, and platelets, all suspended in a complex solution (plasma- approximately 55% of the blood) of gases, salts, proteins (7 g/dl , about 4 g/dl of albumin and 3 g/dl of plasma globulins), carbohydrates, and lipids. It supplies O2 and substances absorbed from the gastrointestinal tract to the tissues, return CO2 to the lungs and other products of metabolism to the kidneys, functions in the regulation of body homeostasis (constancy of the internal environment -temperature, oxygen concentration, pH, ionic composition, osmolarity) and distribute hormones and other agents that regulate cell function. The circulating blood volume accounts for about 7% of body weight.
Origin of heart beat &Electrical Activity of the Heart
The electrical events that originate (automaticity) in the conduction system of the heart initiate orderly (rhythmicity)contraction and relaxation of the chambers of the heart .
In the human heart, the SA node is located at the junction of the superior vena cava with the right atrium. The AV node is located in the right posterior portion of the interatrial septum . There are three bundles of atrial fibers that contain Purkinje type fibers and connect the SA node to the AV node: the anterior internodal tract of Bachman, the middle internodal tract of Wenckebach, and the posterior internodal tract of Thorel. Conduction also occurs through atrial myocytes, but it is more rapid in these bundles. The AV node is normally the only conducting pathway between the atria and ventricles. It is continuous with the bundle of His, which gives off a left bundle branch at the top of the interventricular septum and continues as the right bundle branch. The left bundle branch divides into an anterior fascicle and a posterior fascicle. The branches and fascicles run subendocardially down either side of the septum and come into contact with the Purkinje system, whose fibers spread to all parts of the ventricular myocardium.
The SA node normally discharges most rapidly, depolarization spreading from it to the other regions. This suppresses the intrinsic rhythm of the other pacemaker populations by a mechanism called overdrive suppression. The SA node is therefore the normal cardiac pacemaker, its rate of discharge determining the rate at which the heart beats. The SA node and, to a lesser extent, the AV node, contain small round cells with few organelles, which are connected by gap junctions. These are probably the actual pacemaker cells, and therefore they are called P cells.
SA node – 100 beats / min
AV node – 40-60 beats/min
Bundle of His/Purkinjee fibers: 30-40beats/min
Properties of cardiac cells and Action potentials :
Two main types of action potentials take place in the heart . One type, the fast response (non pace maker action potentials ) , occurs in normal atrial and ventricular myocytes and in the specialized conducting fibers (Purkinje fibers of the heart). The other type of action potential, the slow response (pacemaker potentials ), occurs in the sinoatrial (SA) node, and in the atrioventricular (AV) node.
There are two main differences in the action potentials of cardiac cells Vs neve and muscles :
Self generating
The duration of cardiac action potentials range from 200 to 400 ms. ( Nerves 1ms and muscles 2-5ms)- precludes development of tetany /twitch
The role of calcium ions in depolarization of pacemaker cells as opposed to Na+ in nerves and muscles.
They can be conducted directly from cell to cell
Fast response action potentials : The resting atrial and ventricular myofibers have a transmembrane potential of -90mV. Stimulation produces a propagated action potential that is responsible for initiating contraction. When an action potential is generated, the membrane potential rises above this level in 5 distinct phases, phase 0,1,2,3 and 4.
Phase 0 – The initial rapid depolarization and the overshoot (phase 0) are due to opening of voltage-gated Na+ channels similar to that occurring in nerve and skeletal muscle. This causes the membrane potential to rise at a rate of about 300 V/s. As the membrane voltage rises to about 40 mV sodium channels close due to a process called inactivation.
Phase 1 – The initial rapid repolarization is due to closure of Na+ channels.
Phase 2 – The subsequent prolonged plateau is due to a slower but prolonged opening of voltage-gated Ca2+ channels and at the same time opening of a few fast K+ channels. There is a balance between the centrifugal flow of K+ and the centripetal flow of Ca2+ causing a plateau of length in variables. The plateau phase lasts approximately 100 ms. The Ca2+ current is due mostly to opening of the slower L-type Ca2+ channels.
Phase 3 -Repolarization to the resting membrane potential due to closure of the Ca2+ channels and K+ efflux through various types of K+ channels.
Phase 4 is resting membrane potential. This is the period that the cell remains in until it is stimulated by an external electrical stimulus (adjacent cell).
Slow Response -Pacemaker potentials :
The key to the rhythmical firing of pacemaker cells is that, unlike other cells , these will slowly depolarize by themselves- a phenomena called Automaticity . The membrane potential of pacemaker cells is about -55 to -60 mV.
The AP is smaller than the fast response, phase 0 is long and caused by slow Ca2+-influx, phase 1 is absent, phase 2 is slow repolarisation, and the real repolarisation in phase 3 is due to inactivation of the slow Ca2+-channels and increased K+–outflux. Phase 4 is not horizontal – prominent prepotentials, and the relative refractory period is long, extending well into phase 4.
Phase 4: Characteristic slope of pacemaker cells. Three or more ionic currents mediate this slow diastolic depolarization. (1)Continuous outflow or “leak” of potassium ions, followed by a decrease in potassium permeability over time (2)there is a slow inward flow of sodium , called the funny current (3)as well as an inward flow of calcium calcium current (ICa) due to opening of T channels. This relatively slow depolarization continues until the threshold potential is reached. Threshold is between -40mV and -50mV. When threshold is reached, the cells enter phase 0.
Phase 0 : The upstroke in a pacemaker cell is relatively slow compared to fast response cells, and ICa due to opening of L channels produces the impulse. The amplitude of the AP is also small. Fast sodium channels are absent in the pacemaker cells.
Phase 3: Potassium permeability is increased, and the efflux of potassium slowly repolarises the cell, along with inactivation of sodium and calcium currents.
Spread of Cardiac Excitation :
Depolarization initiated in the SA node spreads radially through the atria, then converges on the AV node. Atrial depolarization is complete in about 0.1 s. Because conduction in the AV node is slow , a delay of about 0.1 s (AV nodal delay) occurs before excitation spreads to the ventricles. From the top of the septum, the wave of depolarization spreads in the rapidly conducting Purkinje fibers to all parts of the ventricles in the 0.08–0.1 s. In humans, depolarization of the ventricular muscle starts at the left side of the interventricular septum and moves first to the right across the midportion of the septum. The wave of depolarization then spreads down the septum to the apex of the heart. It returns along the ventricular walls to the AV groove, proceeding from the endocardial to the epicardial surface . The last parts of the heart to be depolarized are the posterobasal portion of the left ventricle, the pulmonary conus, and the uppermost portion of the septum.
Conduction rates :
SA node – 0.05 m/s
Atrial tissue- 1 m/s
AV node – 0.05 m/s
Bundle of His – 1 m/s
Purkinjee system -4 m/s
Ventricular muscles- 1 m/s
Relation of the action potential to the contractile response- Excitation contraction coupling :
Cardiac excitation-contraction coupling is the process which links electrical excitation of the cardiac myocytes with heart contraction and relaxation. The spontaneous firing from the pacemaker spreads over the entire heart as a propagating wave of excitation that is conducted rapidly along the long axis of a cardiac fibre, and spreads along the myocardial sarcolemma from cell to cell via gap junctions.The excitation also reaches the cells interior through the large T-tubules which invaginate the cardiac fibers at the Z line .
During the phase 2 plateau of the action potential, Ca2+ permeability increases, and Ca2+ flows down its electrochemical gradient into the cell through the slow Ca2+-channels in the sarcolemma and T tubules. The small Ca2+ influx is called trigger-Ca2+, because it releases large amounts of Ca2+ from the sarcoplasmic reticulum, the major source of ionic calcium required for cardiac contraction. Consequently cytoplasmic [Ca2+] increases from the resting level of 10-7 To 10-5. The free Ca2+ binds to troponin C, and the complex interacts with tropomyosin to activate sites between the actin and the myosin filaments. This process starts crossbridge cycling and thus contraction of the myofibrils.
At the end of systole, the Ca2+ influx stops, and the sarcoplasmic reticulum is no longer stimulated to release Ca2+ but avidly takes up Ca2+ by means of an ATP-energized calcium pump. In addition, phosphorylation of troponin I inhibits the binding of Ca2+ to troponin C. This process permits tropomyosin to again block the sites for interaction between the actin and myosin filaments, and relaxation (diastole) occurs
Heart as a Pump
Cardiac Cycle
A cardiac cycle is defined as one complete sequence of contraction (systole) and relaxation(diastole).
Ventricular Systole :
Isovulmetric contraction
Ejection
Ventricular Diastole :
Isovolumic relaxation
Rapid filling phase
Diastasis
Atrial systole
Ventricular Systole :
Ventricular systole begins when the action potential crosses the AV node and sweeps over the ventricular muscle—an event indicated by the QRS complex of the electrocardiogram. The onset of ventricular contraction coincides with the peak of the R wave on an ECG and with the initial vibration of the first heart sound.
Contraction of the ventricular muscle cells causes intraventricular pressure to rise above that in the atrium, which causes abrupt closure of the AV valve.
Pressure in the left ventricle continues to rise sharply as the ventricular contraction intensifies. When the left ventricular pressure exceeds that in the aorta, the aortic valve opens. The period of time between mitral valve closure and aortic valve opening is referred to as the isovolumetric contraction phase because during this interval the ventricle is a closed chamber with a fixed volume.
Ventricular ejection begins with the opening of the aortic valve. In early ejection, blood enters the aorta rapidly and causes the pressure there to rise. Pressure builds simultaneously in both the ventricle and the aorta as the ventricular muscle cells continue to contract in early systole. This period is often called the rapid ejection phase.
Left ventricular and aortic pressures ultimately reach a maximum called peak systolic pressure. At this point the strength of ventricular muscle contraction begins to wane- reduced ejection phase . Muscle shortening and ejection continue, but at a reduced rate. Aortic pressure begins to fall because blood is leaving the aorta and large arteries faster than blood is entering from the left ventricle. Throughout ejection, very small pressure differences exist between the left ventricle and the aorta because the aortic valve orifice is so large that it presents very little resistance to flow.
Eventually, the strength of the ventricular contraction diminishes to the point where intraventricular pressure falls below aortic pressure. This causes abrupt closure of the aortic valve. A dip, called the incisura or dicrotic notch, appears in the aortic pressure trace because a small volume of aortic blood must flow backward to fill the aortic valve leaflets as they close.
At the end of ventricular ejection, a volume of blood approximately equal to that ejected during systole remains in the ventricular cavities. This residual volume- End Systolic Volume. The amount of blood ejected from the ventricle during a single beat, the stroke volume, is equal to ventricular end-diastolic volume minus ventricular end-systolic volume.
After aortic valve closure, intraventricular pressure falls rapidly as the ventricular muscle relaxes. For a brief interval, called the isovolumetric relaxation phase, the mitral valve is also closed. Ultimately, intraventricular pressure falls below atrial pressure, the AV valve opens.
The atrial pressure progressively rises during ventricular systole because blood continues to return to the heart and fill the atrium. The elevated atrial pressure at the end of systole promotes rapid ventricular filling once the AV valve opens.
The rapid ventricular filling phase is followed by a phase of slow ventricular filling called diastasis. During diastasis, blood returning from the peripheral veins flows into the right ventricle, and blood from the pulmonary veins flows into the left ventricle, secondary to their momentum.
The onset of atrial systole occurs soon after the beginning of the P wave (curve of atrial depolarization) of the ECG. This completes the ventricular filling . The contribution of atrial contraction to ventricular filling is governed to a great extent by the heart rate . Should tachycardia become so great that the rapid filling phase is encroached on, atrial contraction assumes great importance in rapidly propelling blood into the ventricle during this brief period of the cardiac cycle.
At a normal resting heart rate of about 70 beats per minute, the heart spends approximately two thirds of the cardiac cycle in diastole and one third in systole. Right atrial systole precedes left atrial systole, and contraction of the right ventricle starts after that of the left ventricle.
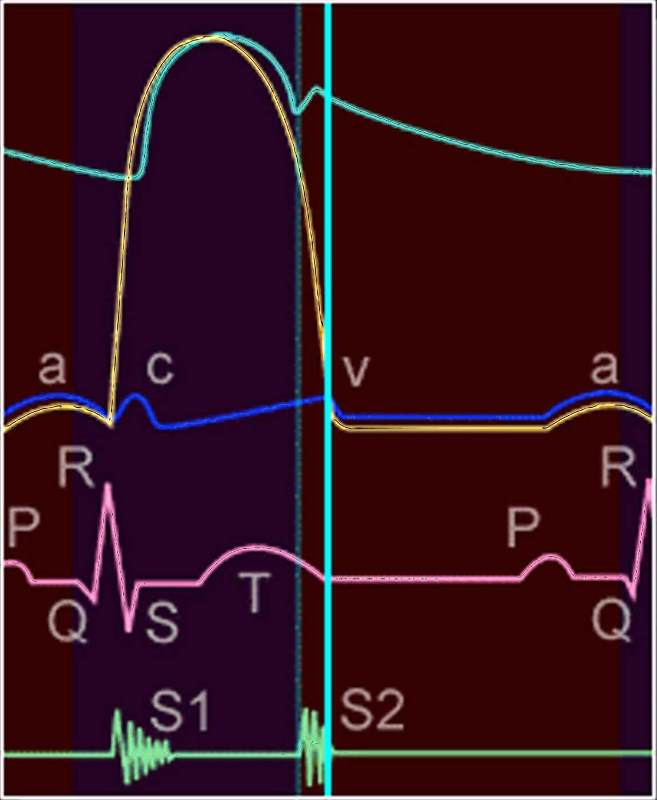
| Pressure Diagram |
| 33808b.800 heart cardiac physiology pressure EKG ECG pressure curves diagram LV aorta LA left atrium left ventricle systole diastole acv waves Davidoff MD |
|
Cardiac Ejection |
| 34814c01.800 heart aorta systole normal physiology function contraction myocardial function ejetion fraction aortic valve mitral valve closed coapted Davidoff art Davidoff MD |
|
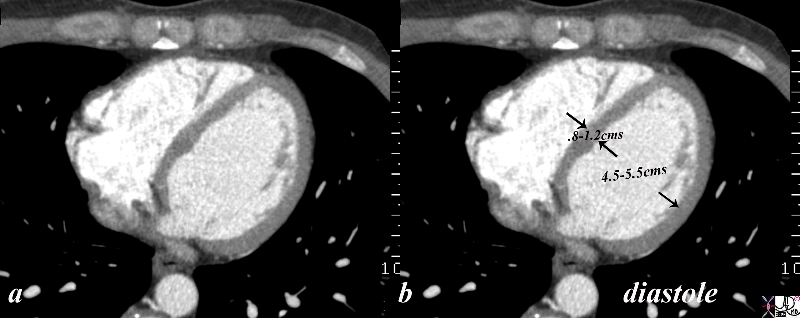
34765c02.8s |
| 34765c02.8s The gated CT scan was taken in diastole and shows the normal left ventriclar dimensions which for the left ventricle wall is between .8cms and 1.2 cms, and for the cavity is 4.5-5.5cms. the measurement should be taken at the level of the paillary muscles which is in mid ventricular cavity. code LV left ventricle papillary muscle cavity free wall septal wall normal anatomy CTscan gated EKG ECG diastole Courtesy Ashley Davidoff copyright 2009 all rights reserved |

Left Heart FAilure |
| 46786c01 heart cardiac pulmonary arteries arteries fx enlarged fx corkscrew interstitial edema LAE left atrial enlargement dx cardiac failure cardiac congestion CTscan Davidoff MD |

Skin CHF |
| 46786c02 skin heart cardiac breast fx left atrial enlargement LAE fx third spacing fx effusions fx skin edema cardiac failure CHF CTscan Davidoff MD |
|
34131s |
| 34131s HEART left ventricle ischemia dyskinesis dysfunction induced by ischemia induced by stress Courtesy Ashley Davidoff MD |
Cardiac output :
The amount of blood pumped from each ventricle of the heart per unit time is the cardiac output. The pulmonary and systemic circulations are arranged in series, ie, one after the other. Consequently, the right and left heart , must each pump an identical volume of blood each minute. This amount is called the cardiac output , and equals 5 to 6 L/min in normal resting individuals.
CO = SV*HR ( Co – cardiac ouput, SV- stroke volume and HR is the heart rate ).
Two methods of measuring output that are applicable to humans, in addition to Doppler combined with echocardiography, are the direct Fick method and the indicator dilution method.
Arterial Pulse :
The blood forced into the aorta during systole sets up a pressure wave that travels along the arteries that expands the arterial walls as it travels, and the expansion is palpable as the pulse. The pulse is felt in the radial artery at the wrist about 0.1 s after the peak of systolic ejection into the aorta.
The aorta distends or balloons out during systole because more blood enters the aorta than leaves it. During diastole, the arterial pressure is maintained by the elastic recoil of walls of the aorta and other large arteries. Nonetheless, aortic pressure gradually falls during diastole as the aorta supplies blood to the systemic vascular beds. The lowest aortic pressure, reached at the end of diastole, is called diastolic pressure. The difference between diastolic and peak systolic pressure in the aorta is called the arterial pulse pressure. Typical values for systolic and diastolic pressures in the aorta are 120 and 80 mmHg, respectively.
Atrial pressure changes & Jugular venous pulse :
The atrial pressure changes are transmitted to the great veins, producing three characteristic positive waves and two negative deflections in the record of jugular pressure.
Positive deflections :
The a wave is due to atrial systole. Some blood regurgitates into the great veins when the atria contract, even though the orifices of the great veins are constricted.
The c wave is the transmitted manifestation of the rise in atrial pressure produced by the bulging of the tricuspid valve into the atria during isovolumetric ventricular contraction.
The v wave mirrors the rise in atrial pressure before the tricuspid valve opens during diastole and represents atrial filling .
Negative deflections :
X decent : is systolic and coincides with the carotid pulse. It represents atrial relaxation.
Y decent : is diastolic and begins after carotid pulse . It represents the rapid filling phase of the ventricle .
Heart Sounds :
The first heart sound (s1) is a low, slightly prolonged “lub” , caused by vibrations set up by the sudden closure of the mitral and tricuspid valves at the start of ventricular systole .
The second heart sound(s2) is a shorter, high-pitched “dup” , caused by vibrations associated with closure of the aortic and pulmonary valves just after the end of ventricular systole.
The third heart sound (s3) is due to vibrations subsequent to rapid ventricular filling . Hear midway through diastole.
The fourth heart sound(s4) is due to early ventricular filing and is heard just before S1.
Regulation of Myocardial Function :
Intrinsic regulation
Extrinsic regulation – Nervous or chemical (hormonal regulation)
Intrinsic regulation :
Two principal intrinsic mechanisms, namely the (1) Frank-Starling mechanism and (2) rate-induced regulation, enable the myocardium to adapt to changes in hemodynamic conditions.
Frank Starling mechanism:
The force of contraction of the cardiac muscle is proportional to its initial length.
Rate induced Regulation :
Myocardial performance is also regulated by changes in the frequency at which the myocardial fibers contract. Transient changes in the intervals between beats profoundly affect the strength of contraction. When the left ventricle contracts prematurely , the premature contraction (extrasystole) itself is feeble, whereas contraction ,postextrasystolic contraction, after the compensatory pause is very strong. Inadequate time for ventricular filling just before the premature beat accounts partly for the weak premature contraction. Subsequently, the exaggerated degree of filling associated with the long compensatory pause explains in part the vigorous postextrasystolic contraction.
Extrinsic Regulation :
Nervous system : Sympathetic and Parasympathetic
Sympathetic : Sympathetic nervous activity enhances atrial and ventricular contractility. Sympathetic nervous activity also enhances myocardial performance by activating calcium channels in myocardial cell membranes. The right sympathetic trunk supplies the SA node and the left supplies the AV node.
Parasympathetic : The vagus nerves inhibit the cardiac pacemaker, atrial myocardium, and AV conduction tissue . The vagus nerves also depress the ventricular myocardium, but the effects are less pronounced in the ventricles than in the atria.
ThYROID HORMONES : thyroid hormones enhance myocardial contractility
Heart Rate
The Common Vein
Copyright 2008
Intrauterine Pulse Rates
The fetal begins beating at a rate near the maternal rate at rest, being about 75-80 beats per minute (bpm). By 7 weeks (LMP week 9) it accelerates to 165-185 bpm, an increase of 100 bpm in the first month. It then decelerates to about 150 bpm at week 13 (week 15 after the LMP), and by term it is about 145 bpm.
There is no difference in male and female heart rates before birth.
| bat | 750 |
| mouse | 530 |
| hamster | 450 |
| rat | 330 |
| guinea pig | 280 |
| chicken | 280 |
| squirrel | 250 |
| rabbit | 205 |
| monkey | 190 |
| skunk | 170 |
| cat | 120 |
| goat | 90 |
| sheep | 75 |
| man | 70 |
| giraffe | 65 |
| ass | 50 |
| horse | 45 |
| lion | 40 |
| elephant | 35 |
| camel | 30 |
Modified from The Merck Veterinary Manual 6th Edition 1986
-
Links and References
-
TCV