Introduction Blood Supply
The Coronary Circulation
Copyright 2020
Introduction
The heart is the only organ that supplies its own circulation. The arteries that supply blood to the heart are the right and left coronary arteries, which take origin from the right and left coronary ostia at the base of the aorta. The blood vessels travel on or just below the epicardial surface and then enter the myocardium at either an oblique angle or at a 90 degree angle. The capillary network is quite extensive and results in a 1:1 ratio of capillary to myofibril which is very high, but is necessary to meet the high metabolic demand of the myofibril and the heart. Capillary density is less in the interventricular septum and AV nodal tissue making them more susceptible to ischemia, putting the conduction systems in these areas at a relatively higher risk to ischemia
About 5% of cardiac output is supplied to the coronary arteries. Blood flow is during diastole, since the myocardium around the intramyocardial vessels is relaxed.
The word coronary arises from the Latin word “corona” meaning crown. The reason for this term is exemplified below.

Corona = Crown or wreath from mid 17th century (in the sense ‘resembling a crown’): from Latin coronarius, from corona ‘wreath, crown’. In the above series A post mortem heart was inflated and injected with barium and the subsequent X -ray was turned upside down so that the apex is pointing straight upward and the base of the heart is inferior, The shape of the heart when oriented this way is much like a crown.
Courtesy Ashley Davidoff MD 07582c11.8bL
The infrastructure of the coronary artery conforms to the cross of scaffolding described in the introduction to the applied anatomy of the heart.

The Cross in 3 Dimensions
The infrastructure of the heart as a cross has horizontal and vertical components that have 3 dimensions (b). The tricuspid valve and annulus (blue ring) and mitral valve and annulus (red horizontal ring) are aligned in the horizontal plane (c). The right coronary artery (RCA) and circumflex (LCx) supply the right and left side while the left anterior descending (LAD) and posterior descending artery (PDA) align along the the vertical limb.
Ashley Davidoff MD
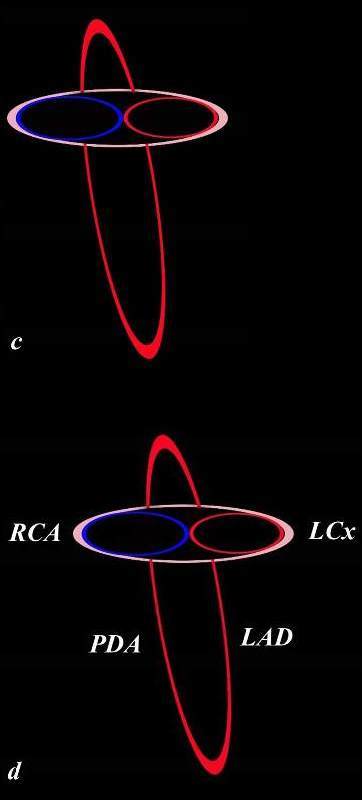
The Cross in 3 Dimensions
The infrastructure of the heart as a cross has horizontal and vertical components that have 3 dimensions.
The tricuspid valve and annulus (blue ring) and mitral valve and annulus (red horizontal ring) are aligned in the horizontal plane (c). The right coronary artery (RCA) and circumflex (LCx) supply the right and left side while the left anterior descending (LAD) and posterior descending artery (PDA) align along the the vertical limb.
Ashley Davidoff MD
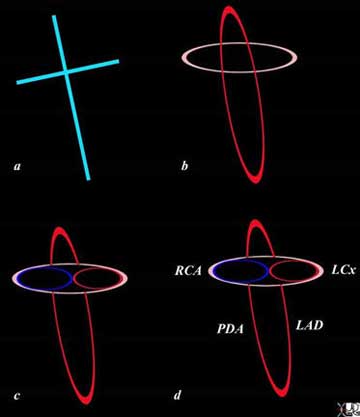
The infrastructure of the heart as a cross, has horizontal and vertical components that have 3 dimensions (b). The tricuspid valve and annulus (blue ring) and mitral valve and annulus (red horizontal ring) are aligned in the horizontal plane (c). The right coronary artery (RCA) and circumflex (LCx) supply the right and left side respectively, while the left anterior descending (LAD) and posterior descending artery (PDA) align along the vertical limb.
Courtesy: Ashley Davidoff M.D.
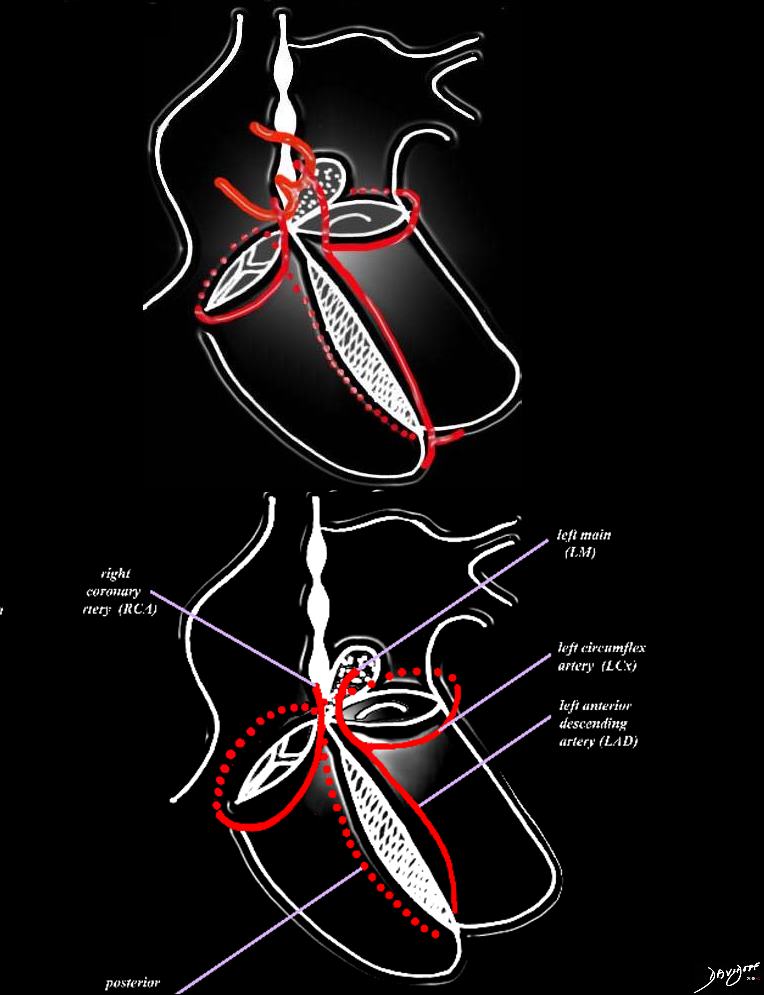
The heart has a left and right arterial system. The vessels are formed around the cross of the heart, “vertically” along the inter ventricular septum and inter atrial septum, and “horizontally” in the atrioventricular (A-V) grooves. The left coronary artery arises from the left coronary ostium and supplies one branch, the left anterior descending artery, that travels anteriorly on the anterior aspect of the inter ventricular septum, and one branch that travels in the atrioventricular groove (left circumflex). The right coronary artery has a branch that courses along the right atrioventricular groove and usually continues as the posterior descending artery on the posterior aspect of the inter ventricular groove, and commonly gives rise to the A-V nodal branch, at the back of the crux of the heart, which travels in the vertical axis in the inter atrial septum.
Courtesy of: Ashley Davidoff, M.D.
The left coronary artery supplies most the left ventricle and septum together with the left atrium. Blood supply to the posterior portion of the heart is highly variable.
The left coronary artery originates from the left coronary sinus which is slightly posterior and superior to the right coronary cusp. After the left main coronary artery branches into the LAD and circumflex, the LAD proceeds in the interventricular groove and supplies the anterolateral aspect of the heart and most of the septum including the anterior fascicle of the left bundle and the right bundle branch. The circumflex proceeds in the left A-V groove first coursing anteriorly and then posteriorly and supplies the posterolateral aspect of the left ventricle to variable extent as well as the left atrium.
The right coronary artery originates from the right coronary sinus. It makes a loop in the anterior groove and then proceeds to the posterior part of the atrioventricular groove, and usually ends as the posterior descending artery in the posterior interventricular groove. Distribution includes the anterior lateral and posterior aspects of the right ventricle, the right atrium and the lower one third of the interventricular septum including the posterior fascicle of the left bundle branch. It often supplies the AV nodal artery (85-90%), the SA nodal artery (60% of cases), and sometimes a portion of the posterior aspect of the left ventricle.
The vessels enter the myocardium from the surface and proceed into the myocardium at variable angles.

Normal Left Coronary Artery
Takotsubo cardiomyopathy 008Vb03 from ashley davidoffon Vimeo.

Courtesy Michael Maysky
Copyright 2009
Normal Right Coronary Artery
Takotsubo cardiomyopathy 008Vb05 from ashley davidoffon Vimeo.
Coronary Dominance
The manner in which the posterior and inferior part of the heart, and more particularly the left ventricle and posterior septum are supplied is quite variable. Sometimes it is dominantly supplied by the RCA and less commonly by the LCA. Coronary dominance defines the vessel that supplies this area of the heart. The classical definition of dominance has been related to which of the two vessels give rise to the posterior descending artery. The right coronary artery feeds the posterior descending artery in 85% of patients and by inference in this context is dominant in 85% of hearts.
However a more useful definition relates to the posterior circulation of the heart that includes the origin of the PDA, the A-V nodal artery and the posterior left ventricular artery. If all these vessels are supplied by the right coronary artery, then it is a right dominant system. If the origin of these three vessels is shared by both vessels, then it is called a co-dominant or balanced circulation.
With this latter definition, the RCA is dominant in 70%, LCA is dominant in 10%, and co-dominance occurs in about 20% of people.
The detail of each of the vessels will be advanced and exemplified in anatomical and angiographic situations.
The Left Coronary Artery
There are three major branches of the LCA;
left main coronary artery.
left anterior descending artery
left circumflex coronary artery

The Left Coronary Artery |
|
The normal coronary arteries of the post mortem specimen have been injected with barium. The heart is projected in the anteroposterior (A-P on the left) and lateral projection. In the AP projection the LAD is seen in the interventricular groove and in the lateral projection the LAD is shown anteriorly and branches of the circumflex are shown posteriorly. Davidoff photography copyright 2009 22390c02scd |
The Left Main Coronary Artery
The left main coronary artery is between 1 and 25mm long, typically about 10-20mm, but can be up to 40mm. It is about 4.5mms in diameter (3-6mm), arises from the left coronary ostium and terminates in the bifurcation into the LAD and circumflex coronary artery. It is best viewed in the A-P projection during angiography. Occasionally it is absent (1%) in which case the LAD and circumflex have separate origins. (Mill) In about 35% of cases there is a trifurcation and the third and middle branch is called the ramus medianus which acts like a first diagonal artery.
The left main proceeds in a leftward direction and courses behind the pulmonary artery and right ventricular outflow tract.

The Left Main Coronary Artery |
|
The angiogram in the anteroposterior projection shows the left main coronary artery overlaid in red, just before it branches into the LAD and circumflex coronary artery. In angiography the A-P view is the best view to identify the full extent of the left main coronary artery The study was performed using Sones technique and the catheter in this instance has slipped out of the ostium after the injection. This technique is rarely used and preformed catheters are preferred. Courtesy Ashley Davidoff copyright 2009 all rights reserved 07034c01.8s |
CT angiography (CTA) allows for the evaluation of the left main coronary artery in any plane. Since the vessel lies posterior to the pulmonary outflow tract, it is necessary to digitally manipulate the image in order to expose left main from the surrounding tissues.

CTA of the Left Main Coronary Artery |
|
The volume rendering of the normal left main coronary artery (red overlay) is seen in image b. The left atrial appendage and right ventricular outflow tract have been digitally removed to expose the left main coronary artery 87255c02.8s Courtesy Philips Medical Systems |
After a short distance the left main terminates usually by bifurcating into the LAD and circumflex vessels.

Left Main Terminates as the LAD and Circumflex |
|
The filet view of the left coronary artery allows one to open the vessels and display them for optimal evaluation. In image b the left main coronary artery has been overlaid in red and the LAD marked as such and the circumflex is seen as the second main division of the LM. The vessels are normal. 87261c02.8s Courtesy Philips Medical Systems |
An example of a ramus medianus (aka ramus branch) is shown below. The ramus acts like a first diagonal artery in the territory it serves.

Trifurcation of the Left Main |
| The coronary angiogram in the LAO projection shows a trifurcation of the left main into the left anterior descending artery, (LAD) ramus medianus, and circumflex coronary artery. The trifurcation is a variant of normal and the ramus supplies the anterolateral aspect of the heart veruy much like a first diagonal would function. code artery heart cardiac coronary artery ramus medianus, and circumflex coronary artery.
Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 07052c02.8s |
The Left Anterior Descending Coronary Artery
The LAD measures about 4mm in diameter proximally, and about 2mm distally. It originates at the bifurcation of the left main and often terminates in characteristic moustache shaped branching pattern at the apex, but often passes around the apex (80%). Less commonly it falls short of the apex and the PDA passes around the apex from the posterior location. The LAD and PDA form an anastomoses at the apex.
In about 4% of patients there are two LAD’s that travel in parallel, with one vessel supplying the septal perforators and the other the diagonals. (Mills)

LAD |
| The normal coronary arteries of the post mortem specimen have been injected with barium. The heart is projected in the anteroposterior (A-P on the left) and lateral projection. In the AP projection the LAD is seen in the interventricular groove and in the lateral projection the LAD is shown anteriorly and branches of the circumflex are shown posteriorly.
Davidoff photography copyright 2008 22390c02scd |
|
Anatomic Specimen Showing the LAD, Diagonals and Portion of the Obtuse Marginals |
|
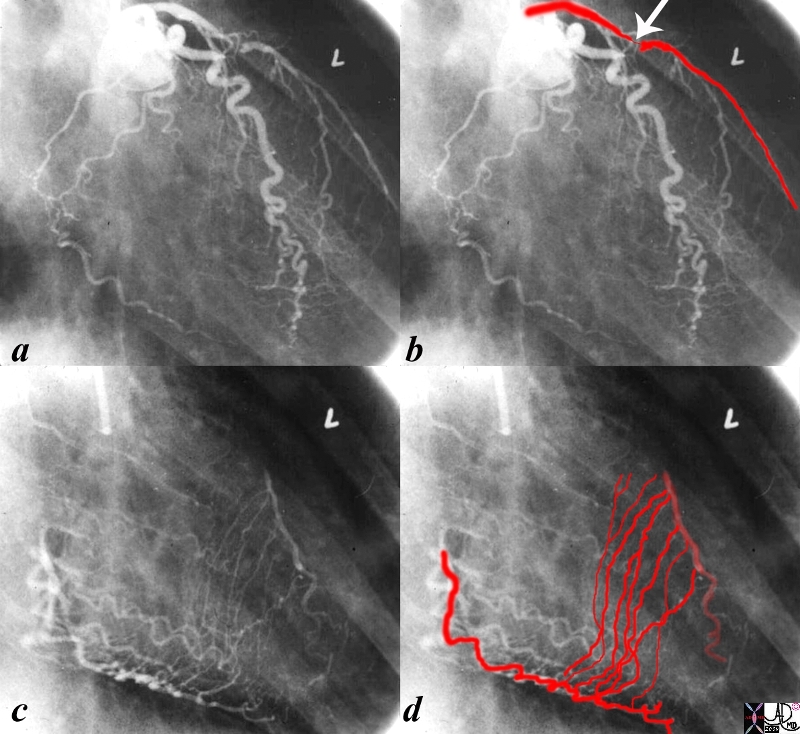
The heart specimen has been injected with barium into the coronary arteries and in this instance the left coronary artery is demonstrated. In image b, the red overlay represents the LAD in the interventricular groove which reflects the position of the interventricular septum. Image c shows the diagonal arteries supplying the anterolateral aspect of the left ventricle. The last image (d ) shows a few branches of the circumflex coronary artery. These vessels will be detailed below. Courtesy Ashley DAvidoff MD copyright 2009 15009cc01.81s |

LAD and its Major Branches |
|
The left coronary angiogram is taken in the left anterior oblique projection showing the left anterior descending artery (LAD) in b (red) and the diagonal branches in c. The septal branches are the other main branches of the LAD and they are shown in d. Courtesy Ashley Davidoff copyright 2009 all rights reserved 15029c07.8s |

The Moustache of the Distal LAD Characteristic but not Always Present |
|
The angiogram is from an infant with hypoplastic left heart syndrome and aortic atresia and shows the classical moustache shape bifurcation of the distal LAD . The catheter course advances from the IVC, through the right atrium, right ventricle, pulmonary artery through a patent ductus arteriosus and into the descending aorta. Since there was no forward flow of blood from the LV because of the aortic atresia, the flow went retrograde to perfuse the ascending aorta and the coronary arteries. The image was taken at the end of the run and forward flow had proceeded thus emptying the distal aorta of contrast and the retrograde flow of contrast into the coronary arteries was still present. Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 00269b04c01.8s |

LAD and the Apex |
|
The left coronary angiogram in the LAO projection shows th distribution of the distal LAD as it proceeds around the apex to the inferior aspect of the apex of left ventricle. The anastomosis with the PDA is not demonstrated. Courtesy Ashley DAvidoff MD copyright 2009 all rights reserved 07052c02.81s |
Conal Artery (aka Vieussen’s Artery)
The first branch of the LAD is a small and barely seen conal artery that together with the right coronary artery supplies the right ventricular outflow tract. This anastomosis is a major collateral pathway when there is a stenosis in the left main, proximal LAD or proximal RCA. The conal artery is also called the artery of Vieussens and is named after the French anatomist Raymond de Vieussens (1641 – 1715)

Conal Artery or Artery of Vieussen’s |
|
The normal coronary arteries of the post mortem specimen have been injected with barium. The heart is projected in lateral projection. The conal artery (aka artery of Vieussens) is the first branch of the LAD and it supplies the right ventricular outflow tract. It collateralizes with the larger counterpart which is a branch of the right coronary artery. It is displayed with red overlay in b and magnified in c. The counterpart branches from the right coronary artery are seen outlined with white barium. Davidoff photography copyright 2008 Courtesy Ashley Davidoff MD 22390.1.5kc05.8s |

Conal Artery |
|
The angiogram in the LAO projection shows the conal artery (aka artery of Vieussens) usually arising as the first vessel off the LAD, but in this instance seems to arise after the first diagonal, although the origin of the vessel may be hidden by the LAD. The anastomosis with the conal branch from the right side is noted at the edge of the upper terminal branch where a small branch of the right sided component of the conal artery is seen. Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 07044c01.8s |
Diagonal Arteries
There are usually 2-6 diagonal branches that travel over the anterolateral surface of the heart and supply this region as well the anterolateral papillary muscle. . The diagonals initially run on the surface of the heart and therefore can be visualized by CT imaging. At variable distances from their origin they gradually dive into the myocardium. The first diagonal is generally the largest branch, but there is a wide variation in size and number of diagonal arteries.
|
Diagonal Arteries Supplying the Anterolateral Aspect of the Left Ventricle
|
|
The normal coronary arteries of the post mortem specimen have been injected with barium. The heart is projected in the anteroposterior (A-P -a,b) and lateral projection (c,d). In the AP projection the LAD is seen in the interventricular groove and in the lateral projection the LAD is shown anteriorly with branches of the circumflex shown posteriorly, and the diagonals noted between these major branches. The diagonals supply the anterolateral aspects of the left ventricle. They are overlaid in red both in their epicardial and their subepicardial distribution (b,d). As they travel on the epicardial surface the white barium is well visualized (a,c) and while they travel subepicardial a shadow of their distribution is noted. They dive into the myocardium at variable distances and at variable angles and become invisible as they traverse the myocardium. Davidoff photography copyright 2009 all rights reserved 22390c02.82sc01.8s |
|
Diagonal Arteries off the LAD |
|
The reconstructed CT image of the normal left coronary circulation from a lateral projection shows the left coronary artery arising from the left aortic cusp starting out as the left main which is a short vessel and not well demonstrated in this view. The diagonals are well demonstrated in this view with distribution to the anterolateral parts of the left ventricle. Courtesy Philips Medical Systems 87260b01.8s |
Septal Perforators
Multiple septal perforators (typically between 4-6 in number) originate at right angles from the LAD, and are directed toward the diaphragm. The first septal artery usually arises just after the first diagonal and it is the largest of the septal arteries. The septal vessels arising from the LAD, supply the upper 2/3rds of the septum. The right bundle and the anterior fascicle of the left bundle are supplied by the LAD perforators. In general the density of the capillaries is reduced in the septum making the conduction system in this area susceptible to ischemia. The lower 1/3rd is supplied by the posterior descending artery and these vessels anastomose seamlessly. The anastomosis allows the perforators to act as a major collateral pathway between the left and right circulation. Thus a significant stenosis in the LAD will result in a lower pressure distally in the vessel and the right coronary artery will be able to supply this area via the septal arteries distal to the stenosis. These collaterals require time to mature and function optimally when the evolution of the stenosis is slow. In the event of an acute mid LAD thrombosis for example, collaterals will usually not be effective.
|
Septal Perforators Off the LAD |
|
The angiogram is performed in the RAO projection and the left anterior descending artery is recognized by the fine septal perforators that supply the upper 2/3 rds of the septum. The direction of the septal perforators is characteristic in that they head toward the diaphragm. The lower 1/3 of the septum is supplied by the septal perforators off the PDA. The septal perforators from the LAD and the PDA form an anastomosis. These vessels are not visualised by CT because they are intramural and very small. The first septal perforator is usually larger than the other septals. Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 06998c.8s |
In angiography multiple projections are required to evaluate stenotic disease. The distinction between the LAD and diagonals and marginals as they cross over each other is sometimes difficult. The septal arteries help characterize the LAD and enable recognition by virtue of their size and direction toward diaphragm.
|
Septal Collaterals |
|
The first angiogram (a,b) is from an injection of the left coronary artery in the RAO projection. A subtotal occlusion in the proximal LAD (arrow) is noted. There is an implied high pressure gradient between the proximal and distal LAD and a predicted low pressure in the distal LAD based on the severity of the stenosis. The second injection (c,d) is into a normal right coronary artery with delayed imaging when most of the contrast has washed out from the upstream portion of the RCA vessel and shows septal collateral vessels supplying the downstream LAD from a high pressure RCA to the low pressure of the distal LAD. Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 15042c02.8s |
Circumflex Coronary Artery
The proximal circumflex artery in a right dominant systems measured about 3.5mms in diameter and is usually about the same size as the proximal LAD. In left dominant systems measured 4mms.
In a right dominant system, it arises as a branch of the left main and terminates as a small vessel in the posterior portion of the heart (85%).
As it starts out it courses under the left atrial appendage to enter the anterior portion of the atrioventricular groove. In general it gives off 3-5obtuse marginal vessels feeding the anterolateral portion of the heart (usually OM1) , the lateral margin– obtuse marginal proper (usually the largest vessel) being second (OM2) and the third (usually OM3) feeding the posterolateral aspect sometimes with smaller branches in between. A posterior left ventricular branch may arise from the circumflex, but it then usually terminates as a small vessel. The number and size of the obtuse marginal vessels is variable.
The obtuse marginals typically supply the posterolateral aspects of the LV as well as the posterolateral papillary muscle.
The circumflex also gives rise to the left atrial branches. In about 40% of individuals it gives rise to the SA nodal vessel, and supplies the A-V node in about 10%.

Circumflex and Obtuse Marginals in a Right Dominant System |
|
The normal coronary arteries of the post mortem specimen have been injected with barium. The heart is projected in lateral projection. The branches of the circumflex coronary artery have been overlaid in red (b) as they supply the lateral and posterolateral portion of the left ventricle. In this case there are at least 4 obtuse marginal vessels with OM4 supplying the “buttocks” of the LV Davidoff photography copyright 2008 Courtesy Ashley Davidoff MD 22390.1.5kc03.8s |
|
Posterior View of the Obtuse Marginals Non Dominant Left Coronary Artery |
|
The posterior aspect of the heart shows a barium injection of the left coronary artery overlaid in red. Image a shows the continuation of the circumflex after it has given off the firs and second obtuse marginal arteries. Image b shows the 3rd and 4th obtuse marginal arteries that supply the lateral and posterior parts of the left ventricle. Since the RCA supplies the PDA, A-V nodal and posterior left ventricular branch this heart has a completely dominant right coronary artery. Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 15008ccc01.83s |
The distal circumflex can be a confusing vessel to define in angiography, since often one of the marginals, usually second, is so large, that the distal true circumflex becomes inordinately small, quite insignificant in appearance, and delayed in opacification. Its position in the later phases of the angiogram in the A-V groove (defined by the later filling of the coronary sinus) allows for its identification.

The Confounding Distal Circumflex in a Non- dominant Left System |
|
The left coronary angiogram is taken in the left anterior oblique projection showing the distal circumflex artery in b as a small tortuous almost insignificant vessel compared to the proximal circumflex. The second marginal (2 in b) is so large that the distal circumflex seems insignificant. Since in this patient the RCA is dominant, the distal circumflex plays a small part in supplying the posterior and inferior portions of the LV. The first obtuse marginal (1) overlaid in red in c, arises from the anterior portion of the circumflex. The second obtuse margina(2) is huge. The 3rd obtuse marginal (3) arises from the posterior portion of the circumflex artery. The last branch is a tiny posterior left ventricular artery. In d two small vessels are shown. The first, off the larger anterior portion is likely the S-A nodal artery and or left atrial branch, and the second arises from the smaller posterior portion and is a small left atrial branch. The left coronary angiogram is taken in the left anterior oblique projection showing the true circumflex artery in b. The anterior (proximal ) component is relatively large compared to the much smaller posterior portion because in this instance the second marginal is so large that the true circumflex seems insignificant. and the distal circumflex does not supply a large portion of the posterior and inferolateral portion of the heart. The first obtuse marginal (1) overlaid in red in c, arises from the anterior portion of the circumflex. The second obtuse marginal (2) is huge. The 3rd obtuse marginal (3) arises from the posterior portion of the circumflex artery. The last branch is a tiny posterior left ventricular artery. In d two small vessels are shown. The first, off the larger anterior portion is likely the S-A nodal artery, and the second arises from the smaller posterior portion and is a small left atrial branch. Courtesy Ashley Davidoff copyright 2009 all rights reserved 15029c11.8s |

Dominant Left Coronary System |
|
The left coronary angiogram in this instance demonstrates a dominant left system. Both the anterior and posterior component of the circumflex, overlaid in red in b, are of a large caliber. In c, the first second third and fourth obtuse marginals are shown. In d the origin of the PDA, posterior left ventricular branch, and the AV nodal artery are shown at the crux of the heart. Since the inferolateral portion of the heart and the A-V nodal artery arise from the left coronary artery it is a left dominant system (about 10% of cases). Courtesy Ashley Davidoff copyright 2009 all rights reserved 06984bc04.8s |
|
CTA – The LCA |
|
The reconstructed CT image of the normal left coronary circulation from a lateral projection shows the left coronary artery arising from the left aortic cusp starting out as the left main which is a short vessel and not well demonstrateed in this view, and dividing in to two main branches – the left anterior descendng artery (LAD) and the circumflex artery (LCX). The LAD provides the anterolateral surface of the LV with diagonal branches, while the circumflex provides the lateral and posterior walls of the left ventricle via the obtuse marginal branches Courtesy Philips Medical Systems 87260b01.8s |
The Right Coronary Artery
The right coronary artery originates from the right coronary sinus. It makes a a half a loop in the the anterior A-V groove and tricuspid valve annulus, and then completes its its second half odf a loop in the posterior part of the atrioventricular groove, usually ending as the posterior descending artery in the posterior interventricular groove.
|
RCA – Anterior View |
|
The heart specimen has been injeted with barium into the coronary arteries and in this instance the right coronary artery is demonstrated. In image b, the red line represents the RCA in the eanterior part of the A-V groove which is hidden deeper in the tissues. Image c showsthe conal artery or the artery of Vieussens supplying the right ventricular outflow tract. The specimen shows many brnches in d that supply the anterior wall of the RV but the only named vessel is the acute marginal artery (arrow) that travels along the right lateral aspect of the right ventricle. Ashley DAvidoff MD copyright 2009 15009b01r04c03.8sb |
|
Posterior and Inferior Surface of the Heart |
|
The posterior aspect of the heart shows a barium injection of the right coronary artery overlaid in red. Image a shows the continuation of the RCA after it has given off the acute right matginal artery . Image b shows the posterior descending artery that riuns along the interventricular groove. Image c adds the posterior left ventricular branch while image d shows the completion of the posterior cross as the atrioventricular nodal artery courses toward the IVC (overlaid in blue. This system is a completely dominant right coronary system since the posterior crux is totally suppied by the RCA Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 15008br05c01 |
|
Branches of the Right Coronary Artery |
|
The coronary angiogram of the RCA is taken in the left anterior oblique projection showing the proximal vessel giving rise to the acute marginal branch (1 in b) and then continues in the posterior aspect of the A-V groove. In c the first branch to be given off is the PDA and then in this instance the vertical small branch is the A–v nodal artery. In d, two posterior LV branches course inferiorly on the posterior aspect of the left ventricle and the last small branch courses cranially to the left atrium as the left atrial branch. Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 07046c03.8s |
The Right Coronary Artery
The proximal right coronary artery (RCA) in a right dominant system is about 4mm and in a left dominant system it is about 3mm. The RCA enters the anterior A-V groove under the right atrial appendage. The first branch is the conus branch, and then multiple unnamed right sided branches supply the anterior wall of the RV.
The acute marginal artery courses along the lateral margin of the RV. Thereafter the RCA courses posteriorly in the A-V groove, and in 85% of patients it gives rise to the posterior descending artery in a typical 90 degree change in direction.
In 60% of patients the RCA gives rise to the SA nodal artery from its anterior portion, and in 90% of patients it gives rise to the A-V nodal artery from its posterior portion. As a completely right dominant system it will supply both the A-V nodal artery and posterior left ventricular artery.

The Right Coronary System |
|
The heart specimen has been injected with barium into the coronary arteries and in this instance the right coronary artery is demonstrated. In image b, the RCA is deep and hidden and the red overlay represents the expected position of the proximal RCA in the anterior part of the A-V groove. Image c shows the conal artery or the artery of Vieussens supplying the right ventricular outflow tract. The specimen shows many branches in d that supply the anterior wall of the RV but the only named vessel is the acute marginal artery (arrow) that travels along the right lateral aspect of the right ventricle (white arrow). Courtesy Ashley Davidoff MD copyright 2009 15009b01r04c03.8sb |

Posterior Right Circulation |
|
The posterior aspect of the heart shows a barium injection of the right coronary artery. Image a shows the continuation of the RCA after it has given off the acute right marginal artery. Image b shows the posterior descending artery that runs along the interventricular groove. Image c adds the posterior left ventricular branches while image d shows the completion of the posterior cross as the atrioventricular nodal artery courses superiorly toward the IVC (overlaid in blue). This system is a completely dominant right coronary system since the posterior crux is totally supplied by the RCA Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 15008br05c01.8s |
|
The Dominant Right Coronary Artery in LAO Projection |
| The coronary angiogram of the RCA is taken in the left anterior oblique projection showing the proximal vessel giving rise in order to the branch to the right ventricular outflow tract (RVOT), acute marginal branch (AM) and then continues in the posterior aspect of the A-V groove. The first branch to be given off is the PDA and then in this instance the vertical small branch is the A-V nodal artery (AVn). Two large posterior LV branches course inferiorly on the posterior aspect of the left ventricle and the last small branch courses cranially to the left atrium as the left atrial branch.
Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 07046c03b02.8s |
|
Right Coronary Artery in RAO projection |
| The injection into the right coronary artery is displayed in the right anterior oblique projection revealing in ordr of branching the sinoatrial nodal artery (SAn) the acute marginal artery (AM) that separates the anterior portion of the RCA in the A-V groove from the posterior portion. The next branch off is the right atrial branch (RA). The RCA takes a hairpin 90 degree turn as it gives off theposterior descending artery ( PDA). The septal perforators (unlabelled) are shown as multiple small vertical branches off the PDA that supply the lower 1/3 of the septum. Note in this patient the PDA curves around to supply the apex – This is uncommon since the LAD usually assumesd this function.
Courtesy Ashley Davidoff copyright 2009 all right reserved 07625c05.8 |
The Conal Artery
The conal artery is the first branch of the right coronary artery and it supplies the right ventricular outflow tract. It collateralizes with its counterpart, the first branch of the LCA. The collateral pathway plays a significant role in patients with evolving hemodynamically significant stenoses in the left main, proximal LAD and proximal RCA lesions.
|
The Conal Artery |
| The normal coronary arteries of the post mortem specimen have been injected with barium. The heart is projected inAP (a,b) and lateral projection (c,d). The conal artery is the first branch of the RCA and it supplies the right ventricular outflow tract. It collateralizes with the smaller counterpart which is a branch of the left coronary artery. It is displayed with red overlay in b and d. The arrows shows a branch of the smaller conal artery arising from the LCA.
Courtesy Ashley Davidoff MD 22390c02sc04.8s |
SA Nodal Artery
In the past it was thought that a single SA nodal artery was present. It is now felt that that there often two sources of SA nodal artery supply and that there are multiple potential routes for the artery to find its way to the SA node. Infarction of the SA node is rare possibly for the reasons stated above. (Kawashima)
|
The SA nodal Artery off the RCA |
| The right coronary artery has been injected into the right coronary artery and displayed in the right anterior oblique projection and it shows a prominaent SA nodal artery arising as the first vessel off the RCA. The vessel also supplies the right atrium itself.
Courtesy Ashley Davidoff copyright 2009 all rights reserved 07571bc01.8s |
Acute Marginal Artery
The marginal branch of the right coronary artery, follows the right acute margin of the right ventricle and supplies branches to both the anterior and posterior surfaces of the right ventricle. In angiography it helps define the anterior from the posterior aspects of the AV groove.
|
The Acute Marginal Artery |
| The right coronary artery has been injected and displayed in the right anterior oblique projection The acute marginal artery is the largest of the branches of the first anterior ventricular branches and it marks the border between the anterior and posterior wall of the right ventricle.
Courtesy Ashley Davidoff copyright 2009 all rights reserved 07571bc03.8s |
Posterior Descending Coronary Artery
The posterior descending artery marks the posterior border of the interventricular septum and originates by taking a typical 90 degree turn down toward the interventricular septum. It is smaller than the LAD, usually falls short of the apex but anastomoses with the distal LAD which usually supplies the apex. The PDA sometimes has an early takeoff from the right coronary artery before it reaches the crux of the heart. It occasionally supplies the apex . It usually supplies the posterior fascicle of the left bundle conduction system. It often branches off the posterior RCA before it reaches the apex, and rarely it duplicated. It is distinguished from the posterior left ventricular branches by the septal arteries which originate at 90 degrees from the PDA.
|
Posterior Descending Artery |
| Both coronary arteries have been injected with barium in this post mortem specimen. The PDA is shown in red as it takes a 90 degree turn off the right coronary artery. Note the acute marginal artery (AM) reflects the edge of the right side of the heart, and the obtuse marginal off the LCA and circumflex rflects the left edge of the heart. The PDA reflects the inferior border of the heart. The septal perforators supply the posterior and inferior 2/3 of the ventricular septum and arise at right angles off the PDA
Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 07582c07b04.8s |
Septal branches of the Posterior Descending Artery
The posterior descending artery supplies vasculature to the lower 1/3 to 1/4 of the interventricular septum, which anastomoses with the branches arising from the LAD. They arise at right angles off the PDA. They supply the post fascicle of the left bundle branch.
A-V Nodal Artery
The A-V nodal artery is a branch of the posterior and distal portion of the right coronary artery in 90% of patients and arises at the posterior crux of the heart, formed by the distal RCA, that often continues to the left side to branch into posterior left ventricular branches, the A-V nodal artery that proceeds cranially, and the posterior descending artery that proceeds inferiorly. In 10% of patients the AV node is supplied by the left coronary system. The AV node is situated just anterior to the coronary sinus at the entrance of the IVC.
|
The A-V nodal Artery |
| The coronary arteries of the normal heart specimen have been injected with barium and theposterior aspect of the heart in the region of the crux is exposed. The distal circulation of the RCA is overlaid in red in b revealing the distal right coronary artery (RCA), the origin of the AV nodal artery, posterior descending artery (PDA) and the posterior left ventricular branches. Inimages c and d the posterior wall of the right atrium has been lifted and the extent of the AV nodal artery magnified and exposed. The opening of the IVC is ringed in blue
Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 15007cd06.8s |
AV block is associated wit acute myocardial infarctions involving the right coronary artery.
Posterior Left Ventricular Branches (aka Posterolateral Arteries)
The supply of the posterior aspect of the left ventricle is variable and may arise from the left coronary or right coronary system, or from a combination.
|
Angiogram of the Posterior Left Ventricular Branches |
| The coronary angiogram of the RCA is taken in the left anterior oblique projection showing the proximal vessel giving rise in order to the branch to the right ventricular outflow tract (RVOT), acute marginal branch (AM) and then continues in the posterior aspect of the A-V groove. The first branch to be given off is the PDA and then in this instance the vertical small branch is the A-V nodal artery (AVn). Two large posterior LV branches course inferiorly on the posterior aspect of the left ventricle and the last small branch courses cranially to the left atrium as the left atrial branch.
Courtesy Ashley Davidoff MD copyright 2009 all rights reserved 07046c03b02.8s |
Applied Anatomy
Atherosclerosis is a degenerative disorder of the vascular wall characterised by a fibrofatty deposition (plaque) in the inner lining of the artery.
It is the most common disorder of the coronary arteries and a challenging disease to Western cultures particularly because of the high prevalence of the disease and the associated high morbidity and mortality that attends the disease. Atherosclerosis is a normal aging phenomenon but is accelerated in genetically predisposed individuals and is associated with common diseases such as diabetes and hypertension.
The accumulation of plaque in the wall causes narrowing of the lumen of the arteries progressively restricting flow. In addition, the normal smooth and glistening lining of the arteries are replaced by a rough irregular inner wall that is a factor that predisposes to thrombosis, sometimes an acute life threatening event if the arteries of the heart or brain are affected.
The clinical presentation depends on the organ involved and the degree of narrowing. In the heart for example simple narrowing results in chest pain called angina. When total acute obstruction occurs with thrombosis of the artery, severe unremitting chest pain occurs, and myocardial infarction ensues.
The coronary arteries are essentially end arteries and their branching pattern is tree like so that a specific area of the myocardium is essentially only supplied by one mother vessel. As implied in the text, the presence of collaterals, best defined in the conal arteries and septum are available. These however usually require time to mature these collaterals in order that they can compensate for physiological demands at rest and excercise. In an acute coronary thrombosis in a young patient with little atherosclerosis, the collateral system often fails because the collateral system is innately ill equipped to respond to this situation.
Cause: It occurs as a normal course of aging, but it is accelerated by genetic, dietary and behavioral factors.
ResultDiagnosis: The clinical presentation depends on the organ involved and the degree of narrowing. In the heart for example simple narrowing results in chest pain called angina. When total acute obstruction occurs with thrombosis of the artery, severe unremitting chest pain occurs, and myocardial infarction ensues.Each organ has varied manifestations of clinical presentation, all relating to reduced perfusion of the end organ due to narrowing. Imaging plays an essential role in diagnosis. Ultrasound can directly view the lumen and wall of accesible vessels, while CTscan and MRI are advancing to be the mainstay of diagnosis for the deeper arteries. Angiography was the gold standard of the past, is still used and is invaluable in selected circumstances, particulalrly if therapeutic intervention is needed.
|
Atherosclerosis |
| This image shows three pathological specimens of the aorta. In the first image minimally raised fatty streaks are noted. (a). In image b, the fibrous capsule causes raised fibrofatty nodules, while in c, there gas been rupture of the plaques, with friable atheromatous plaques abound.
Courtesy Henri Cuenoud MD 13420c CVS artery aorta atheroscleosis atheroma fatty streaks fibro-fatty plaque |
The proximal RCA was the most common site of symptomatic atherosclerosisDisease in the Left Coronary Artery
|
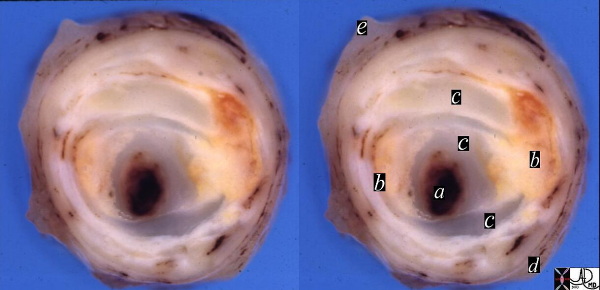
Normal Coronary Artery in Cross Section |
| The normal right coronary artery of a pediatric patient has been opened and the lumen and wall have been exposed. The section has been magnified in b and c and shows a widely patent lumen (red) and a thick muscular wall. (light pink) exemplified in c.
Courtesy Ashley Davidoff Copyright 2009 all rights reserved 07619c02.8s |
|
Stenosis of the Coronary Artery |
|
In this post mortem specimen a thrombus has occluded the narrowed lumen (a) in the presence of cholesterol plaque (b) and fibrous changes and capsule (c) a thinned media (d), and adventitia (e). 13410c Courtesy Henri Cuenoud MD |
Coronary Stenosis
Coronary stenosis is causes by progressive accumulation of atherosclerotic burden in the wall of the vessels resulting in progressive stenosis. Stenosis of greater than 70% is hemodynamically significant. In the left main, a 50% stenosis is clinically relevant. The plaque is variably composed of acute inflammatory changes, fatty cholesterol deposits, fibrous capsules and calcium.
Angiography and more recently CTscan and MRI are able to define the stenotic lesions.

Severe Stenosis of the Left Circumflex |
| The coronary angiogram in the LAO projection shows a severe proximal stenosis (about 70%) of the circumflex with some post stenotic dilatation. The second image has a green overlay indicating the region of disease with the post stenotic dilatation. Courtesy Ashley Davidoff MD.
07023c code heart artery coronary circumflex stenosis atherosclerosis imaging radiology angiography overlay |

Calcified Plaques in the Right Coronary Artery |
|
Filet view of the right coronary artery using CT technology and curved reformatting revealing calcific plaque disease . CT is the study of choice for the evaluation for calcific atherosclerotic disease 44247 Courtesy Ashley Davidoff MD Copyright 2009 |
Coronary Thrombosis
Coronary thrombosis is an acute occlusive process of the coronary artery, almost universally in the presence of atherosclerotic disease resulting in a variety of syndromes commonly presenting with acute chest pain.

Coronary Thrombosis and Thrombolysis |
|
The first image (a) shows a coned down LAO projection of the LAD in a patient with acute thrombosis of the left anterior descending artery. In the second image the thrombus in the artery is overlaid in maroon (b). Following thrombolysis(c) minimal irregularity of the endothelium is seen(arrow d). This may be residual thrombus or reflect the soft tissues of a plaque rupture. Courtesy Ashley Davidoff MD copyright 2009 1695602.8s |
Takotsubo cardiomyopathy 008Vb03 from ashley davidoff on Vimeo.