-
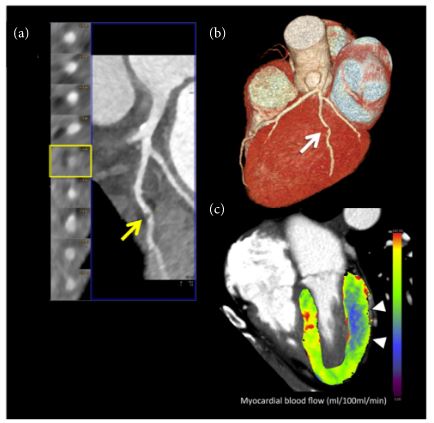
Dynamic CTP imaging. 67-year-old obese female patient with history of hyperlipidemia and smoking with suspected coronary artery disease. (a) Curved multiplanar reformation of coronary CT angiography data showed eccentric noncalcified plaque of the main obtuse marginal branch (OM) causing focal critical stenosis (>70% luminal narrowing), arrow. (b) Three-dimensional volume-rendering reconstruction confirmed the severe coronary artery stenosis of the OM (arrow). (c) Three-dimensional color-coded 4-chamber CT perfusion map image derived from the time-resolved dynamic acquisition during stress with the shuttle mode shows extensive perfusion defects in the territory of the OM (basal-middle lateral wall), color-coded in blue, arrowheads. The colors of the myocardium are coded according to the flow values with red, green, and yellow representing higher flow values than blue. The corresponding value of the hemodynamic parameters derived from the time-attenuation curves (TACs) demonstrates a significant reduction of myocardial blood flow in the territory of the OM, consistent with inducible ischemia. Absolute myocardial blood flow was 61.6 mL/100 mL/min and 118.2 mL/100 mL/min in the OM and remote myocardium (septal wall) territories, respectively.
Seitun S, et al CT Myocardial Perfusion Imaging: A New Frontier in Cardiac Imaging
BioMed Research International / 2018 Article ID 7295460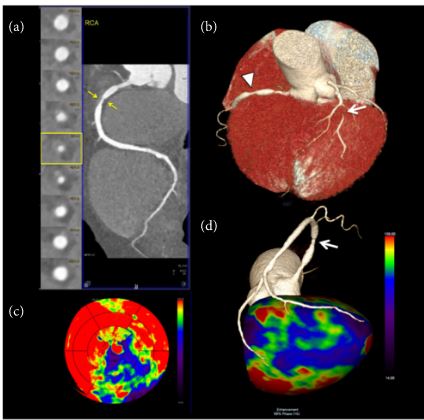
Static single-energy CTP imaging. 61-year-old male patient with multiple cardiovascular risk factors (smoke, hypercholesterolemia, and hypertension) presented with recurrent atypical chest pain. (a) Coronary CT angiography curved multiplanar reconstruction of the right coronary artery (RCA) with the corresponding orthogonal views showed a critical stenosis (>70% luminal narrowing) at the proximal segment sustained by a large noncalcified atherosclerotic plaque with positive remodeling (arrows). (b) Three-dimensional volume-rendering reconstruction demonstrating the critical stenosis of the proximal RCA (arrowhead) and showing also a tight stenosis (>90%, arrow) of the main diagonal branch (arrow). (c) 17-segment polar plot display of CT perfusion data acquired with a prospectively ECG-triggered high-pitch spiral technique at stress during the first pass, arterial phase, showed large, and severe perfusion defect color-coded in violet/blue/green at the inferior and inferolateral wall; note also a severe area of hypoperfusion in the apical lateral segment and in the apex. (d) Three-dimensional volume-rendering modeling of the left ventricular myocardial perfusion data with superimposed coronary tree (inferior view) showed the critical stenosis of the proximal segment of RCA (arrow) associated with an extensive perfusion defect at the inferior and inferolateral wall extending to apex (color-coded in violet/blue/green).
Seitun S, et al CT Myocardial Perfusion Imaging: A New Frontier in Cardiac Imaging
BioMed Research International / 2018 Article ID 7295460 - CT exams take about 20 minutes
- perfusion analysis software measure the amount of contrast present in the myocardium at various stages of the cardiac cycle. Contrast attenuation maps are created, which can be plotted on a bulls-eye or overlaid on anatomical, multi-planar images of the left ventricle. These color maps show the amount of iodine (and thus the amount of blood) in the tissue. Areas of low contrast attenuation match areas of poor perfusion due to ischemia or infarct, similar to the radiotracer sugar uptake by heart cells during nuclear exams.
- With 256- and 320-slice CT scanners, the entire heart can be captured at once. With lower-slice systems, especially the more common 64-slice scanners, the table must move into two positions, back and forth, over several seconds to obtain 10-15 datasets to create a complete cardiac cycle acquisition. These images must then be stitched together. “Real perfusion studies need to be dynamic to show the flow of blood – or contrast in this case – washing in and out of tissue,”
- Radiation dose. “The dose was not acceptable, because of imaging over 30 seconds and needing two tests for both rest and stress,”
- The sensitivity of CT perfusion has been near 100 percent, and it has a high negative predictive value
- myocardial CT perfusion
- imaging technique
- based on myocardial contrast material uptake
- during first arterial pass acquisition.
- The distribution of contrast material is dependent on arterial blood supply, thus allowing myocardial perfusion defects to be detected as areas of low contrast attenuation
- both
- static
- CT MPI can be derived from routine coronary CT angiography studies acquired for the morphologic assessment of CAD
- can be performed using single-energy or dual-energy CT
- only enables qualitative or semiquantitative myocardial evaluation
- sensitivity of 50%–96% for static CT MPI
- specificities of 68%–98%
- dynamic CT myocardial perfusion imaging (MPI)
- cannot be used for the evaluation of coronary arteries
- must be performed in addition to coronary CT angiography,
- typically with use of pharmacologic stress agents, which increase the complexity of this procedure. Although dynamic CT MPI involves a
- higher radiation dose
- allows performing both
- quantitative and
- semiquantitative evaluation of the myocardium
- analysis of the derived time-attenuation curves,
- sensitivity of 76%–100%
- specificities of 74%–100%,
- both static and dynamic CT MPI
- have potential to provide a
- comprehensive anatomic and
- functional evaluation of the heart within a single modality.
- have potential to provide a
- Both enable morphologic and functional assessment of CAD with
- high accuracy and in a
- truly quantitative fashion
- CT MPI as an ancillary test to coronary CT
- restricted to experienced centers.
- Recently, several additional techniques for functional CT assessment of CAD effects on myocardial blood flow have been introduced. These are all based on image postprocessing analysis of standard coronary CT angiography studies: Transluminal attenuation gradient (TAG) is defined as the contrast opacification gradient along the length of a coronary artery at coronary CT angiography and can be directly calculated from in-lumen contrast medium (61). It has been argued that TAG evaluation may be limited by the temporal uniformity that is disrupted by multiple heartbeat acquisitions and its susceptibility to conditions that influence blood flow, such as vessel branching and CAD (62). Therefore, correction models have been developed to overcome possible imprecision in TAG evaluation (61). Corrected coronary opacification is based on the dephasing of contrast material delivery by relating coronary attenuation to corresponding descending aorta opacification in the same transverse plane (63,64). Corrected coronary opacification is then defined as the quotient of this value derived from proximal and distal reference areas of a coronary stenosis. TAG and corrected coronary opacification show a wide spread in reported diagnostic accuracy for detecting hemodynamically significant CAD, with ranges of sensitivity and specificity of 37%–95% and 76%–97%, respectively (3,61,63,65–69). The wide range in diagnostic accuracy is thought to be related to factors that influence image quality, which is a prerequisite for appropriate TAG evaluation. These factors include heavy calcifications, severe CAD, body mass index, and the cardiac phase selected for image acquisition or reconstruction. Beyond this shortcoming, manual TAG and corrected coronary opacification evaluation is rather time consuming, which to date limits its applicability in a real-world clinical setting.More recently, the determination of lesion-specific ischemia from coronary CT angiography data by using fractional myocardial mass, a concept of vessel-specific subtended myocardial mass that could reduce anatomic-physiologic mismatch, has been introduced. Fractional myocardial mass is computed by using an approach based on allometric scaling between length of the coronary artery tree and left ventricular myocardial mass (70). Kim et al investigated the diagnostic performance of fractional myocardial mass for the evaluation of lesion-specific ischemia in 724 vessels in 463 patients (71). On a per-vessel level, they demonstrated superior discriminatory power for the ratio of fractional myocardial mass per minimal lumen diameter (FMM/MLD) when compared with diameter stenosis on ICA to detect myocardial ischemia (C-statistics 0.84 vs 0.74, P < .001). The optimal cut-off value of FMM/MLD was 29 g/mm with a sensitivity and specificity of 75% and 77%, respectively. These authors’ preliminary approach, adding myocardial mass to anatomic stenosis, may further reduce the gap between anatomic and physiologic stenosis severity.
- Noninvasive derivation of coronary FFR from diagnostic coronary CT angiography (FFRCT) studies is the most recent approach making a strong bid to match the unmet need for a single imaging test that provides both structural and functional information (72–74). The ability to reliably obtain such combined information in a noninvasive fashion has potential to replace the traditional combination of tests required for appropriate, guideline-driven patient management and assume the role of the long-sought gatekeeper to invasive catheterization and revascularization (45). The concepts, current evidence, clinical integration, and future directions of FFRCT will be discussed in the following sections.
- CT MPI as an ancillary test to coronary CT
- typically with use of pharmacologic stress agents, which increase the complexity of this procedure. Although dynamic CT MPI involves a
- static
Links and References
- Tesche C et al Coronary CT Angiography–derived Fractional Flow Reserve RadiologyVol. 285, No. 1 2017
- Seitun S, et al CT Myocardial Perfusion Imaging: A New Frontier in Cardiac Imaging BioMed Research International / 2018 Article ID 7295460
- 1. Desai. “Cardiac CT beyond Coronary Angiography: Current and Emerging Non-Coronary Cardiac Applications.” Heart 2011; 97:417e424. doi:10.1136/hrt.2009.1843822. Marcus et al. “Myocardial Perfusion Imaging by CT: Today and Tomorrow.” Int J Clin Pract, Oct. 2011, 65 (Suppl. 173), 14–22 doi:10.1111/j.1742-1241.2011.02786.x3. Weininger et al. “Adenosine-stress dynamic real-time myocardial perfusion CT and adenosine-stress first-pass dual-energy myocardial perfusion CT for the assessment of acute chest pain: Initial results.” EurJRadiol 2010, doi:10.1016/j.ejrad.2010.11.022
4. Techasith et al. “Stress Myocardial CT Perfusion An Update and Future Perspective.” JACC Vol. 4, No. 8, 2011 DOI:10.1016/j.jcmg.2011.04.017
5. Ho et al. “Stress and Rest Dynamic Myocardial Perfusion Imaging by Evaluation of Complete Time-Attenuation Curves With Dual-Source CT.” J. Am. Coll. Cardiol. Img. 2010; 3;811-820 doi:10.1016/j.jcmg.2010.05.009
6. Bamberg et al. “Detection of Hemodynamically Significant Coronary Artery Stenosis: Incremental Diagnostic Value of Dynamic CT-based Myocardial Perfusion Imaging.” Radiology: Vol. 260: No. 3, Sept. 2011, doi:10.1148/radiol.11110638/-/DC1
7. Feuchtner et al. “Adenosine Stress High-Pitch 128-Slice Dual Source Myocardial Computed Tomography Perfusion For Imaging Of Reversible Myocardial Ischemia: Comparison with Magnetic Resonance Imaging.” Circ Cardiovasc Imaging, 2011 DOI: 10.1161/CIRCIMAGING.110.961250
