Pulmonary Hypertension
Copyright 2008
Definition
Pulmonary hypertension is a circulatory characterized by an abnormally high pressure in the pulmonary arteries. The diagnosis is defined as a systolic pressure that is greater than 30 mmhg or a mean pressure that is greater than 20 mmhg.
There are many causes for the disorder including, left heart failure, mitral valve disease, chronic lung disease, (cor pulmonale) and left to right shunts. Patients with chronic thromboembolic disease may have hypertension and acute embolic disease may be associated with acute hypertension. When the cause is known it is called secondary hypertension. In many the cause is unknown in which case it is called primary pulmonary hypertension. In some some cases there is a genetic predisposition.
Clinically the entity results and manifests in shortness of breath, coughing, wheezing, chest pain, fatigue, fainting, dizziness, lightheadedness, and swelling in the legs. The diagnosis is confirmed by identifying an enlarged right ventricle, abnormally loud P2 sound, a systolic ejection murmur, and perhaps a pulmonary diastolic murmur, by electrocardiography which shows right ventricular hypertrophy. Echocardiography can not only evaluate right ventricular and right atrial size, but can accurately estimate the pulmonary arterial pressure if there is tricuspid regurgitation. While the CXR CT scan and MRI can evaluate pulmonary arterial size and right ventricular size, the most accurate evaluation of the entity is via cardiac catheterization which measures the pressures directly. Treatment is directed to the cause when known, usually with medication, and oxygen. In patients with underlying mechanical causes such as left to right shunts a surgical option is possible if the fixed component of the hypertension is not excessive.
Normal MPA on CXR
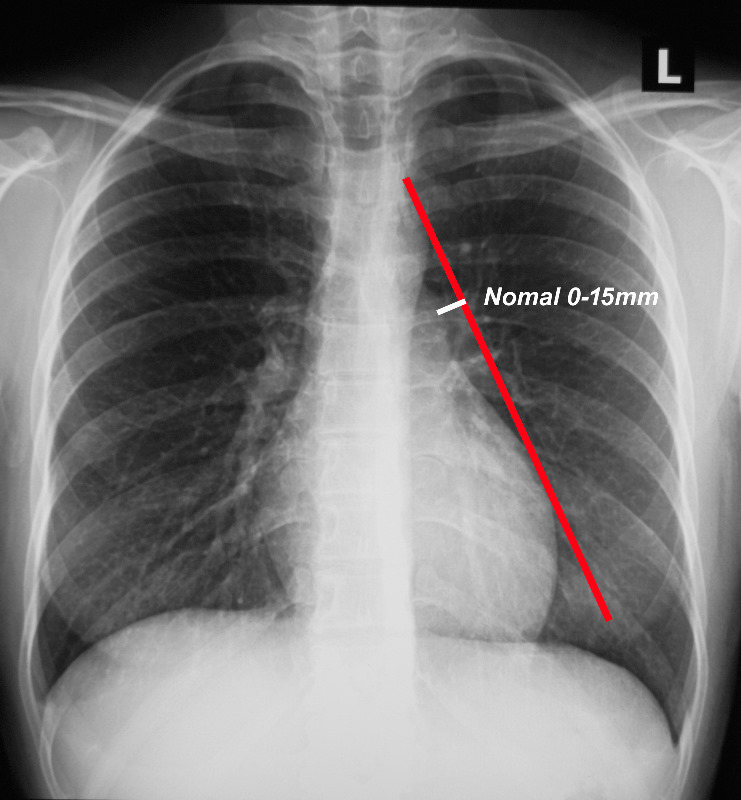
When a line is drawn from the aortic knob to the left edge of the heart, (red line) the pulmonary artery should lie medial to that line (ie along the line drawn to 1.5cms medial to the line)
Ashley Davidoff MD TheCommonVein.net
Pulmonary Hypertension on CXR
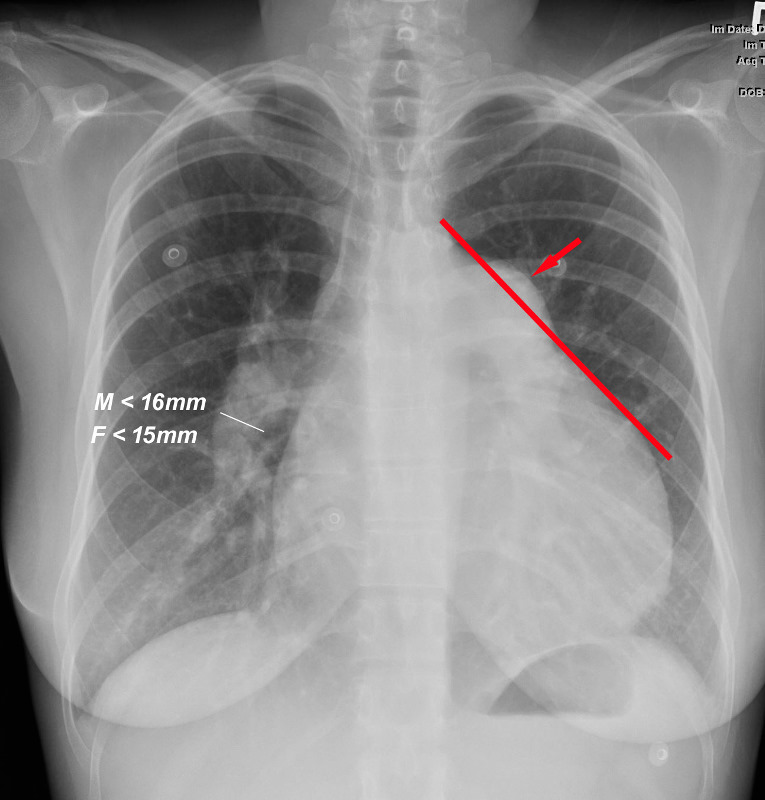
When a line is drawn from the aortic knob to the left edge of the heart, (red line) the pulmonary artery lies lateral to that line indicating an enlarged pulmonary artery most commonly caused by hypertension . In this instance the size of the descending right pulmonary artery is greater than 15 mms confirming the presence of pulmonary hypertension
Ashley Davidoff MD TheCommonVein.net
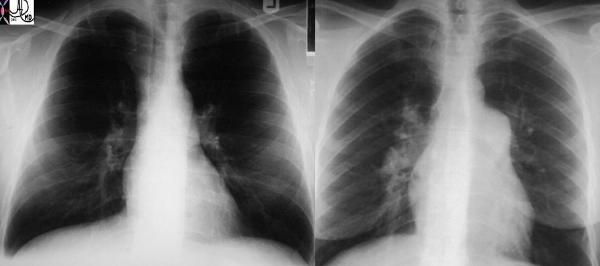
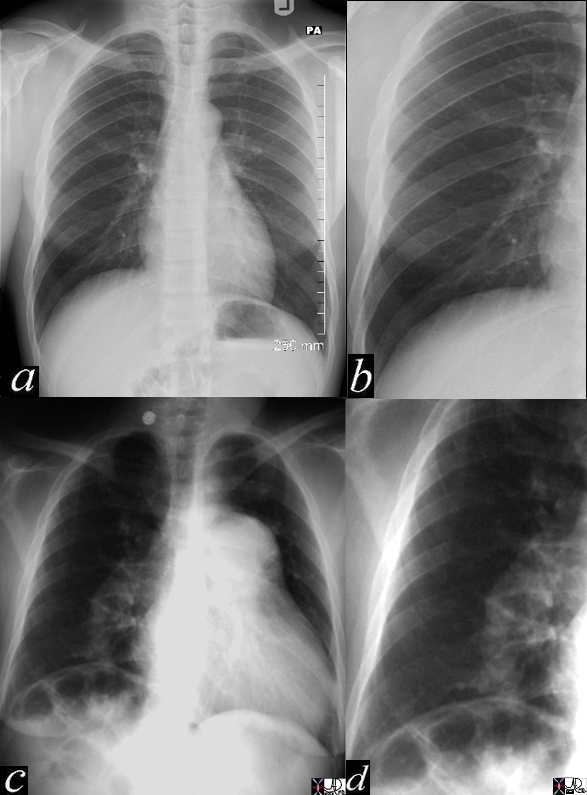
Normal and Pulmonary Hypertension |
| These two P-A chest X-rays show a normal cardiomediastinal image on the left and an enlarged MPA and RPA on the right in this patient with pulmonary hypertension. Courtesy Ashley Davidoff MD (22089 c) code lung main pulmonary artery MPA RPA large hypertension heart cardiac imaging plain film CXR |
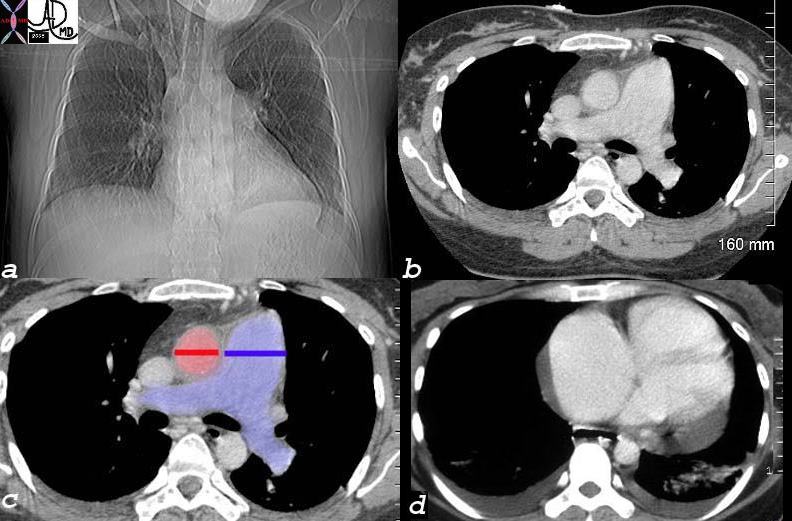
Pulmonary Hypertension – Scleroderma |
|
This unfortunate 32 year old female with scleroderma has many causes for chest pain but the cause under discussion is a relatively uncommon cause for chest pain – pulmonary hypertension. This is best diagnosed with echocardiogram or cardiac catheterization but in this CT the large pulmonary artery (blue – which should be the same size of the red aorta normally) is indicative of pulmonary hypertension. Her heart is enlarged (a) and she has a pericardial effusion, and bilateral pleural effusions (d) both of which can cause pain. In addition she has an enlarged patulous esophagus (seen as a black slit behind the heart (d) characteristic of scleroderma, and associated with reflux which is another cause for chest pain. 30464c12 32 female lungs pleura heart cardiac RA RV right ventricle right atrium pericardium esophagus ILD basal interstitial lung disease pericardial effusion pleural effusion cardiomegaly enlarged esophagus patulous esophagus gallbladder wall edema congestive cardiac failure RHF right heart failure right ventricular enlargement RVE RAE right atrial enlargement pulmonary hypertension cor pulmonale dx scleroderma Courtesy Ashley Davidoff MD |
Normal and Pruning |
| 15406c05 heart cardiac right ventricle RV fx enlarged MPA main pulmonary artery fx enlarged pulmonary arteries DD ASD VSD PDA septal defects Eisenmenger’s CXR plain X-ray of chest Davidoff MD fx pruned pruning dx Eisenmenger’s Davidoff MD 15406.800 15406c02 15406c04 15406c05 |
Pruning of the pulmonary arteries occurs as a result of the remodeling process in response to the increased pressure. The exact mechanisms underlying this pruning are not fully understood, but there are several factors that contribute to it:
- Smooth muscle cell proliferation: The smooth muscle cells in the walls of the pulmonary arteries can undergo abnormal proliferation, leading to thickening of the vessel walls. This thickening narrows the lumen of the arteries, reducing blood flow.
- Endothelial dysfunction: The endothelium, which is the inner lining of the blood vessels, plays a crucial role in maintaining vascular health. In pulmonary hypertension, the endothelial cells can become dysfunctional, leading to impaired production of substances that promote vasodilation and inhibition of smooth muscle cell proliferation. This dysfunction contributes to the narrowing of the pulmonary arteries.
- Inflammatory processes: Chronic inflammation in the pulmonary arteries can further contribute to vascular remodeling. Inflammatory cells and mediators can cause damage to the vessel walls and promote the proliferation of smooth muscle cells, leading to narrowing and pruning of the pulmonary arteries.
The pruning of the pulmonary arteries in pulmonary hypertension has significant implications. The narrowing of the arteries increases resistance to blood flow, making it harder for the heart to pump blood through the lungs. This increased workload on the heart can eventually lead to right ventricular hypertrophy (thickening of the right ventricle of the heart) and right heart failure.
It’s important to note that pulmonary hypertension is a complex condition with various underlying causes, and the severity and specific mechanisms of vascular remodeling can vary among individuals. Treatment approaches for pulmonary hypertension aim to manage the increased pulmonary artery pressure, improve symptoms, and slow down the progression of the disease. These may include medications to dilate the pulmonary arteries, reduce inflammation, or target other specific pathways involved in the pathogenesis of pulmonary hypertension.
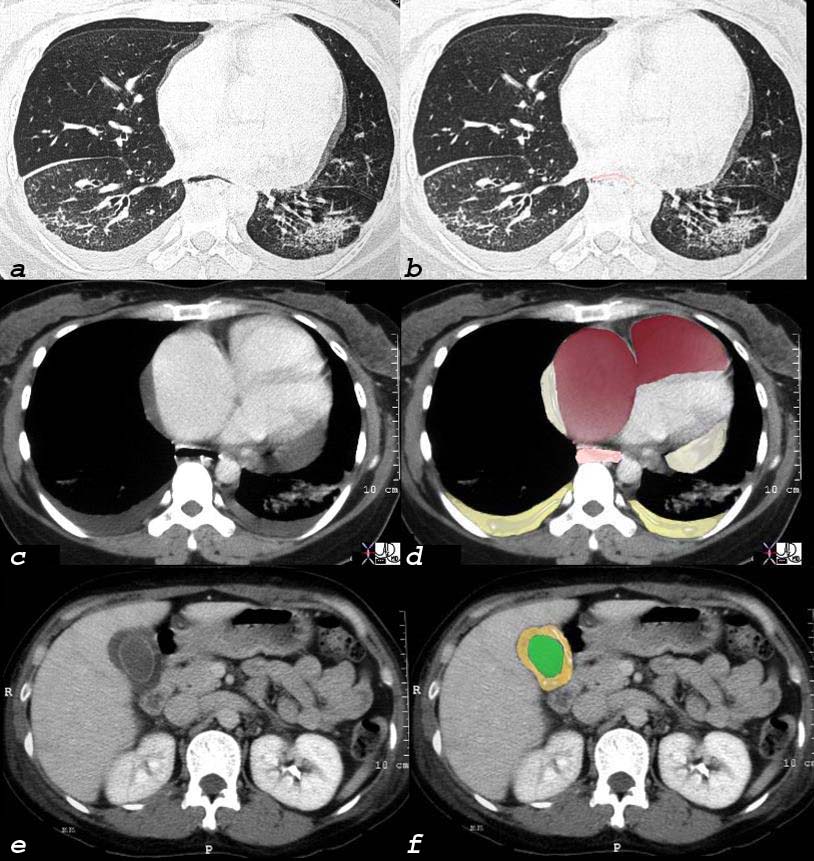
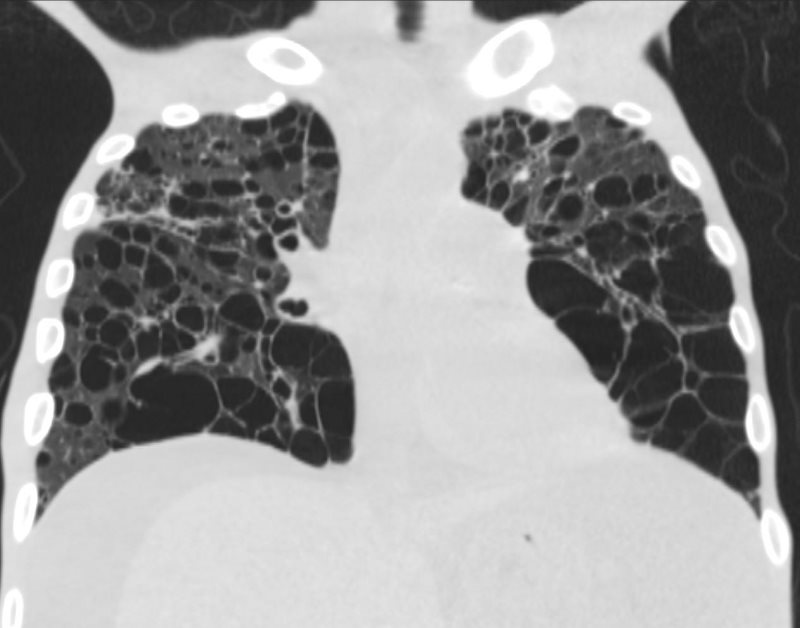
Scleroderma Pulmonary Hypertension and Right Heart Failure |
|
This 32 year old female has scleroderma and her disease is characterized by interstitial basal lung disease (a,b) with normal anterior lung fields and fibrotic posterior lung fields, enlargement of right heart structures (maroon in d), pericardial effusion (light yellow in d), pleural effusions (dark yellow in d) and an edematous wall (orange, in f) of the gallbladder (lumen is green). As a result of her lung disease she developed pulmonary hypertension, right heart failure and tricuspid regurgitation and this lead to the gallbladder edema. and 30464c08 32 female lungs pleura heart cardiac RA RV right ventricle right atrium pericardium gallbladder esophagus ILD basal interstitial lung disease pericardial effusion pleural effusion cardiomegaly enlarged esophagus patulous esophagus gallbladder wall edema congestive cardiac failure RHF right heart failure pulmonary hypertension cor pulmonale dx scleroderma CT scan Courtesy Ashley Davidoff MD |
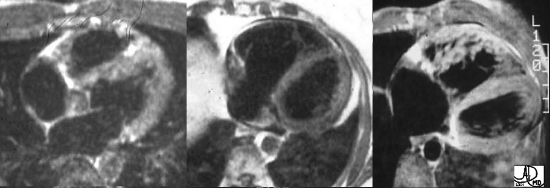
Normal, Dilated, and Hypertrophied Right Ventricles |
| These three images represent T1 weighted images of the RV reflecting normal, dilated, and hypertrophied conditions. Normal thin-walled capacious RV (1) ASD (Atrial Septal Defect) with volume overloaded – thin-walled but dilated RV (2) Pressure overloaded , hypertrophied RV, with accentuated trabeculations (3) Courtesy of Ashley Davidoff M.D. 32095 |
Some Cases
Emphysema and Pulmonary Hypertension
71-year-old female presents with history emphysema
Chest X-ray shows hyperinflated lungs with flattened hemidiaphragms and increase in the retrosternal space and right ventricular enlargement based on the decrease in the retrosternal air space
CT scan confirms the presence of centrilobular emphysema, predominantly in the upper lobes with associated right atrial, right ventricular and pulmonary arterial enlargement. The LA and LV are normal
These findings are consistent with cor pulmonale and pulmonary hypertension, secondary to emphysema.


These findings are consistent with cor pulmonale and pulmonary hypertension, secondary to emphysema.
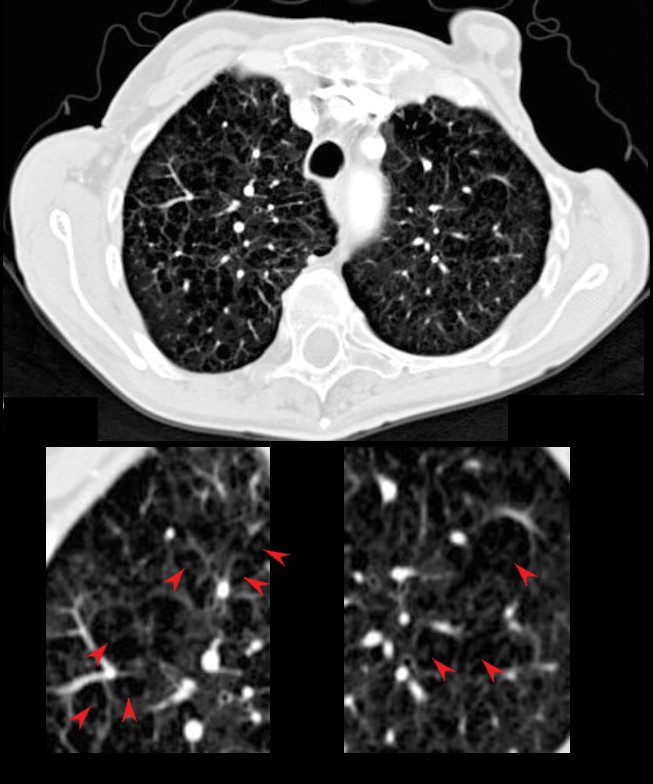
The red arrows point to the soft tissues of the centrilobular emphysema consisting of the arterioles and bronchiolar walls (not usually visible.
71-year-old female presents with history emphysemaAshley Davidoff MD

Ashley Davidoff MD

Ashley Davidoff MD
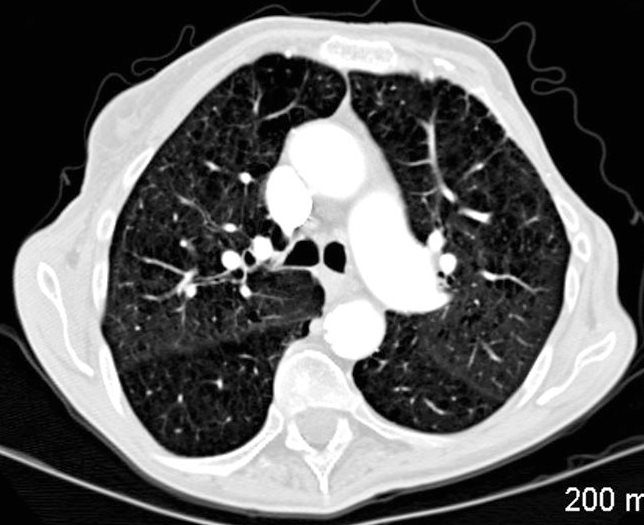
Ashley Davidoff MD

EMPHYSEMA, COR PULMONALE and PULMONARY HYPERTENSION
Ashley Davidoff MD
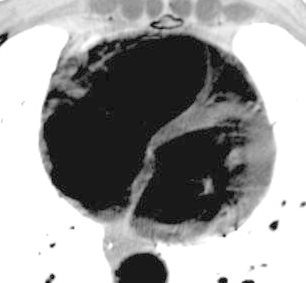
EMPHYSEMA, COR PULMONALE and PULMONARY HYPERTENSION
Ashley Davidoff MD

EMPHYSEMA, COR PULMONALE and PULMONARY HYPERTENSION Ashley Davidoff MD
EMPHYSEMA, COR PULMONALE and PULMONARY HYPERTENSION
Ashley Davidoff MD
SLE and Pulmonary Hypertension
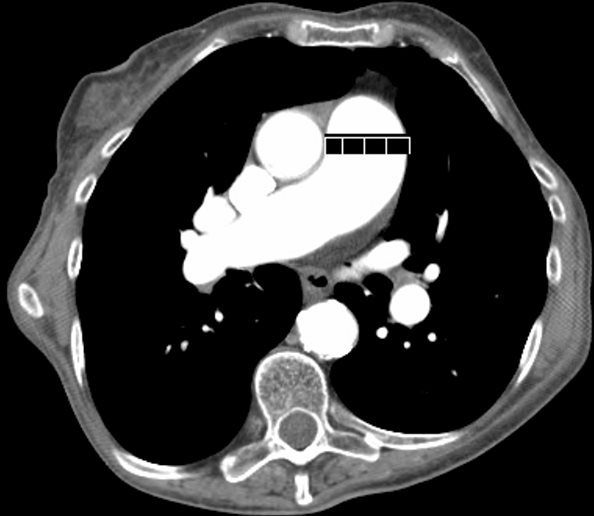
27-year-old female presents with dyspnea and a past history of SLE, Raynaud’s disease, and Lupus nephritis.
Chest X-ray shows cardiomegaly with right ventricular configuration on the PA and an enlarged main and probably left pulmonary and an enlarged descending RPA. The lateral confirms the enlarged RV and raises the possibility of LV enlargement.

SLE and PULMONARY HYPERTENSION without ILD
Ashley Davidoff MD

SLE and PULMONARY HYPERTENSION without ILD
Ashley Davidoff MD
The CT scan confirms an enlarged MPA, RPA, RA and RV, and shows calcification on the posterior leaflet of the mitral valve consistent with Libman Sacks vegetation. There is mild ground glass opacity at the lung bases but no sign of ILD.
A current non contrast abdominal CT shows a pericardial effusion and normal sized kidneys

Ashley Davidoff MD

SLE and PULMONARY HYPERTENSION without ILD
Ashley Davidoff MD

Ashley Davidoff MD

SLE and PULMONARY HYPERTENSION without ILD
Ashley Davidoff MD
LIP HIV?AIDS and Pulmonary Hypertension
27 year old male with a history of perinatal HIV with intermittent highly active antiretroviral therapy (HAART) compliance with a CD4 count of < 50 with biopsy confirmed B cell lymphoma of the liver, s/p CHOP therapy , chronic esophageal strictures s/p dilatations, esophageal candidiasis, LIP, bronchiectasis pancreatitis, and portal vein and splenic vein thrombosis.
Initial Chest X-ray shows a diffuse reticular pattern with cystic changes dominant at the bases.

LIP HIV AIDS and LYMPHOMA
Ashley Davidoff MD
CT at that time confirmed the presence of diffuse cystic changes with the largest cysts at the lung bases. Ascites and splenomegaly are also present
He presented one month later with fever and neutropenia.
CT showed an abscess cavity in the right upper lobe in the right upper lobe, thickened distal esophagus with edematous wall, atrophic gastritis and ascites. Bronchovascular thickening along a bronchiectatic segment in the right upper lobe was present in the last CT
LIP HIV AIDS and LYMPHOMA
Ashley Davidoff MD

LIP HIV AIDS and LYMPHOMA
Ashley Davidoff MD
References and Links
eMedicine Secondary Hypertension Sat Sharma MD
eMedicine Primary Hypertension Ronald Oudiz MD
